Nephrology: Clinical
Nephrology 2: CAKUT/Genetic Clinical and Basic Science
269 - Antibiotic Prophylaxis Practices and Outcomes in Children with Genitourinary Anomalies
Publication Number: 269.251

Sowdhamini S. Wallace, DO, MS (she/her/hers)
Associate Professor of Pediatrics
Texas Children's Hospital
Houston, Texas, United States
Presenting Author(s)
Background:
Antibiotic prophylaxis is associated with a decreased risk of recurrent urinary tract infections (rUTIs) in children with vesicoureteral reflux (VUR). For children with genitourinary (GU) anomalies, survey-based studies of pediatric urologists highlight variations in prescribing practices for prophylaxis, yet data are lacking regarding actual clinical practice patterns.
Objective: 1) To describe the proportion of children receiving antibiotic prophylaxis by GU anomaly type among children presenting to the emergency department (ED) for UTI and 2) compare the frequency of rUTIs in children with and without prophylaxis.
Design/Methods:
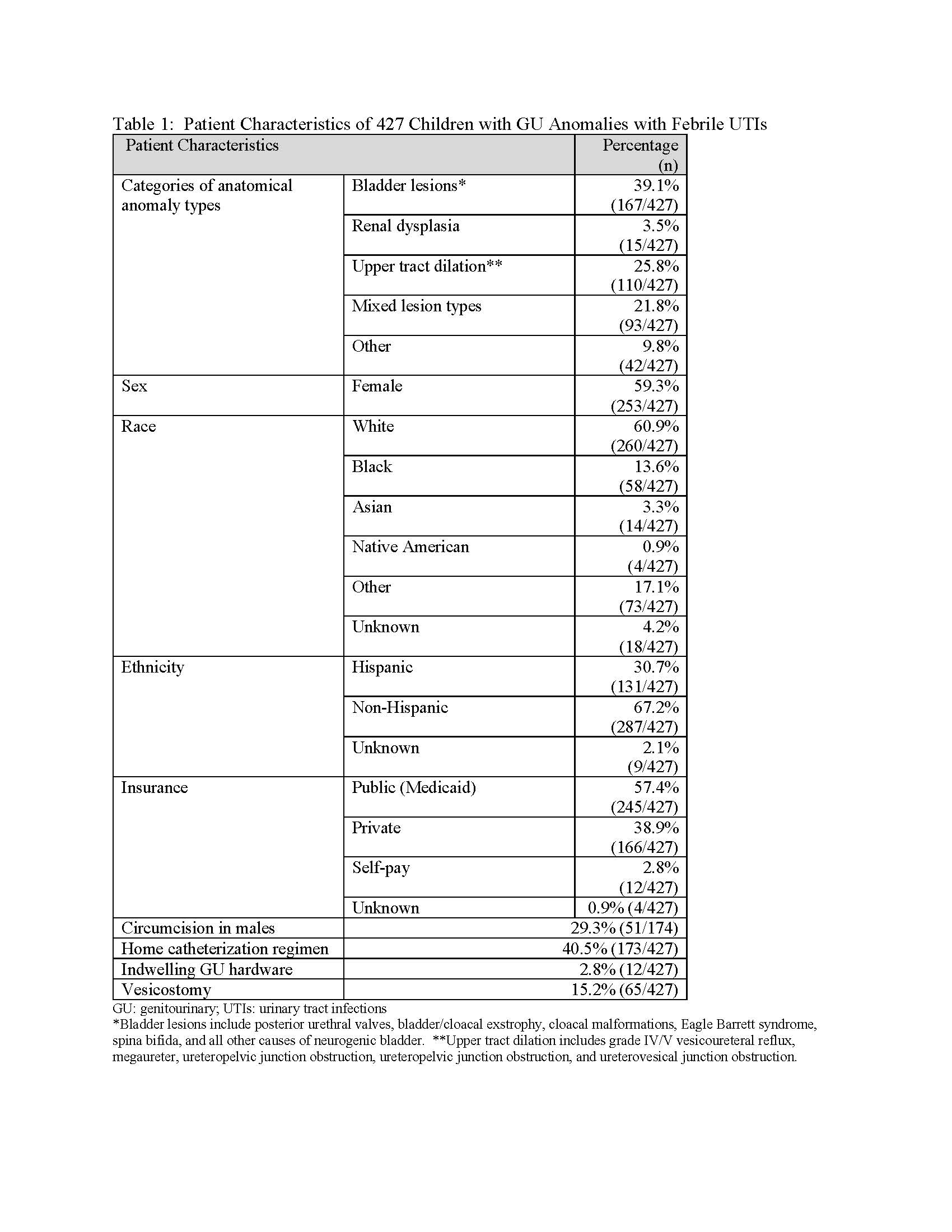
This is an a priori-defined secondary analysis of data collected from a multicenter retrospective cohort of children seen in EDs of 6 free-standing US children’s hospitals from 1/1/2017-12/31/2018. We included unique encounters of children 0-17 years old with neurogenic bladder, obstructive uropathies, renal dysplasia, duplication, and/or high-grade VUR who had a physician-diagnosed febrile UTI. We excluded children with isolated grade I-III VUR anomalies or with end-stage renal disease. We categorized anomalies as: bladder lesions, renal dysplasia, upper tract dilation, mixed anomaly types, or other. The primary outcome was the proportion of children on antibiotic prophylaxis by anomaly type. The secondary outcome was rUTIs during the study period, which was defined as ≥1 subsequent UTIs during the study period. Descriptive and inferential statistics were utilized to describe population characteristics and compare outcomes.
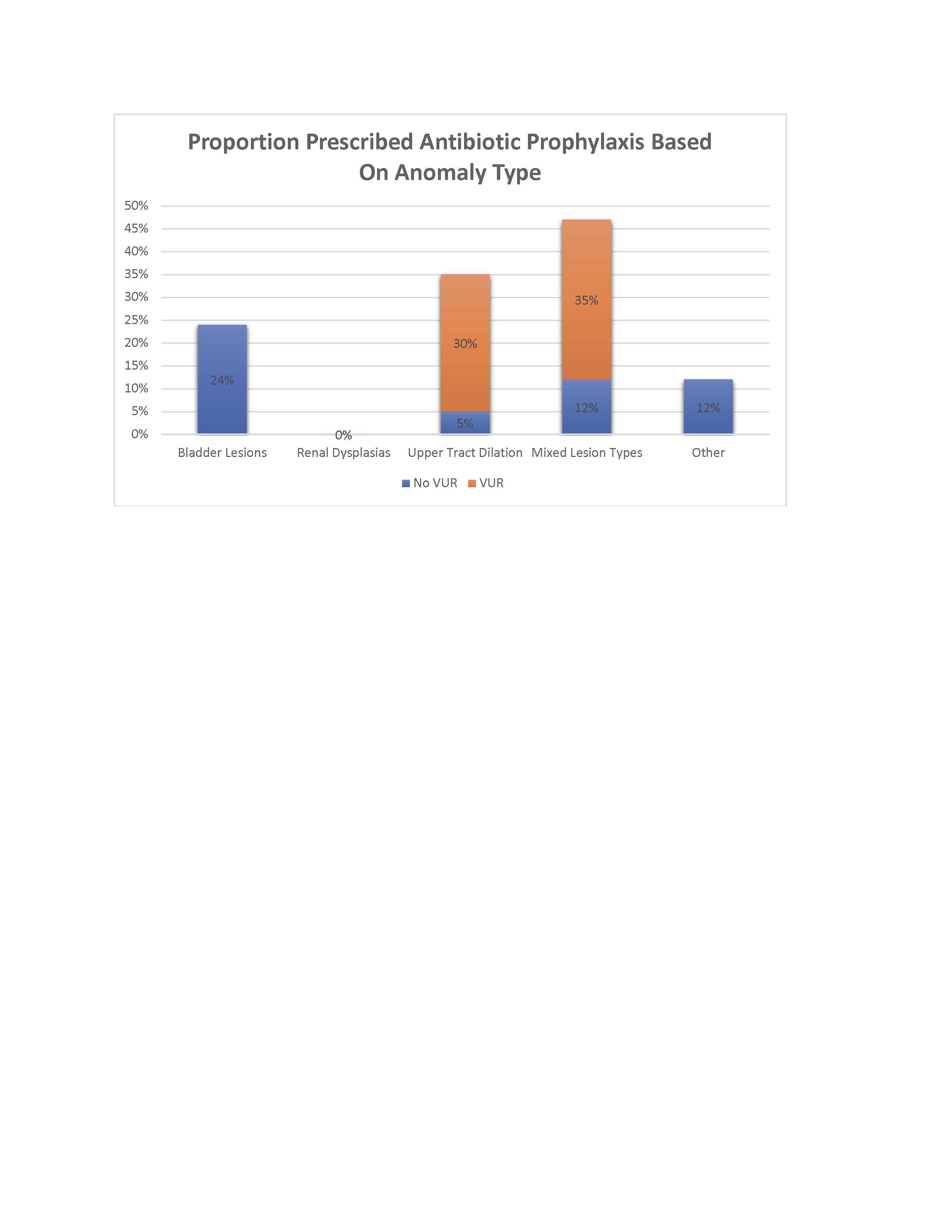
Results: We included 427 unique children. Mean age was 5.6 years (SD 5.3); most had bladder lesions, upper tract dilation, or mixed GU anomaly types [Table]. A minority of children (n=127, 29.7%) were on antibiotic prophylaxis. Prophylaxis regimens included nitrofurantoin (n=53, 41.7%), trimethoprim-sulfamethoxazole (n=46, 36.2%), amoxicillin (n=10, 7.9%), and intravesical gentamicin (n=10, 7.9%). Proportion of children receiving prophylaxis varied by anomaly type, ranging from 0% to 47.3% of children receiving prophylaxis within each anomaly category (p< 0.001) [Figure]. Most children receiving antibiotic prophylaxis in the upper tract dilation and mixed anomaly groups had concomitant VUR. Children presenting to the ED receiving antibiotic prophylaxis had similar risks of rUTIs compared to those without prophylaxis, 39/127 (30.7%) vs. 75/300 (25.0%), respectively (p= 0.22).
Conclusion(s): Prescribing practices of antibiotic prophylaxis varied by anomaly type. When excluding concomitant VUR, the variation was greatest for isolated bladder lesions.