Neonatal Hematology & Bilirubin Metabolism
Neonatal Hematology & Bilirubin Metabolism 2: Hematology
136 - Characteristics of red blood cell transfusion among very preterm infants in China
Publication Number: 136.239

LU ZHENG
fellow
Children’s Hospital of Fudan Univeristy
shanghai, Shanghai, China (People's Republic)
Presenting Author(s)
Background: National-level data on the incidence of RBC transfusions among very preterm infants(VPIs)in China are lacking.
Objective: The objective of this study was to the use and variation of RBC transfusion among VPIs China.
Design/Methods: This cohort study was conducted comprising 57 tertiary hospitals in 2019 and 70 hospitals in 2020 from 25 provinces throughout China. All infants with gestational age (GA) less than 32 weeks who were admitted to the NICUs between January 1 2019 to December 31, 2020, were included. Infants with incomplete treatment in NICUs or with major congenital anomalies were excluded. Readmissions and transfers between participating hospitals were tracked as data from the same infants. Infants were followed until NICU discharge/transfer or death.
Results:
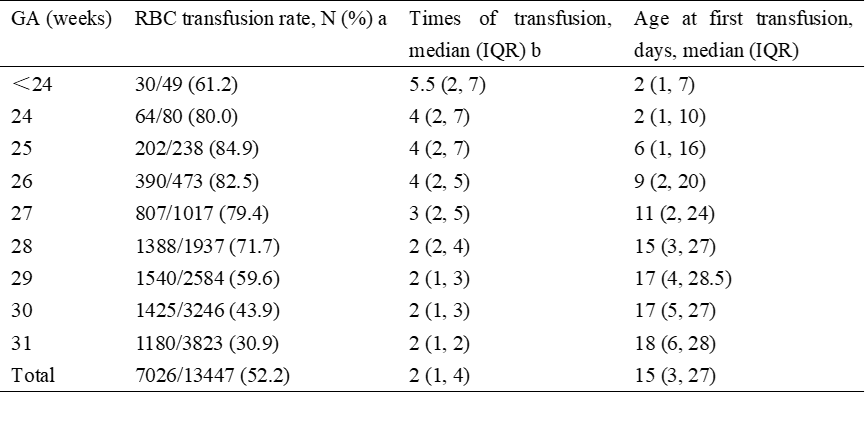
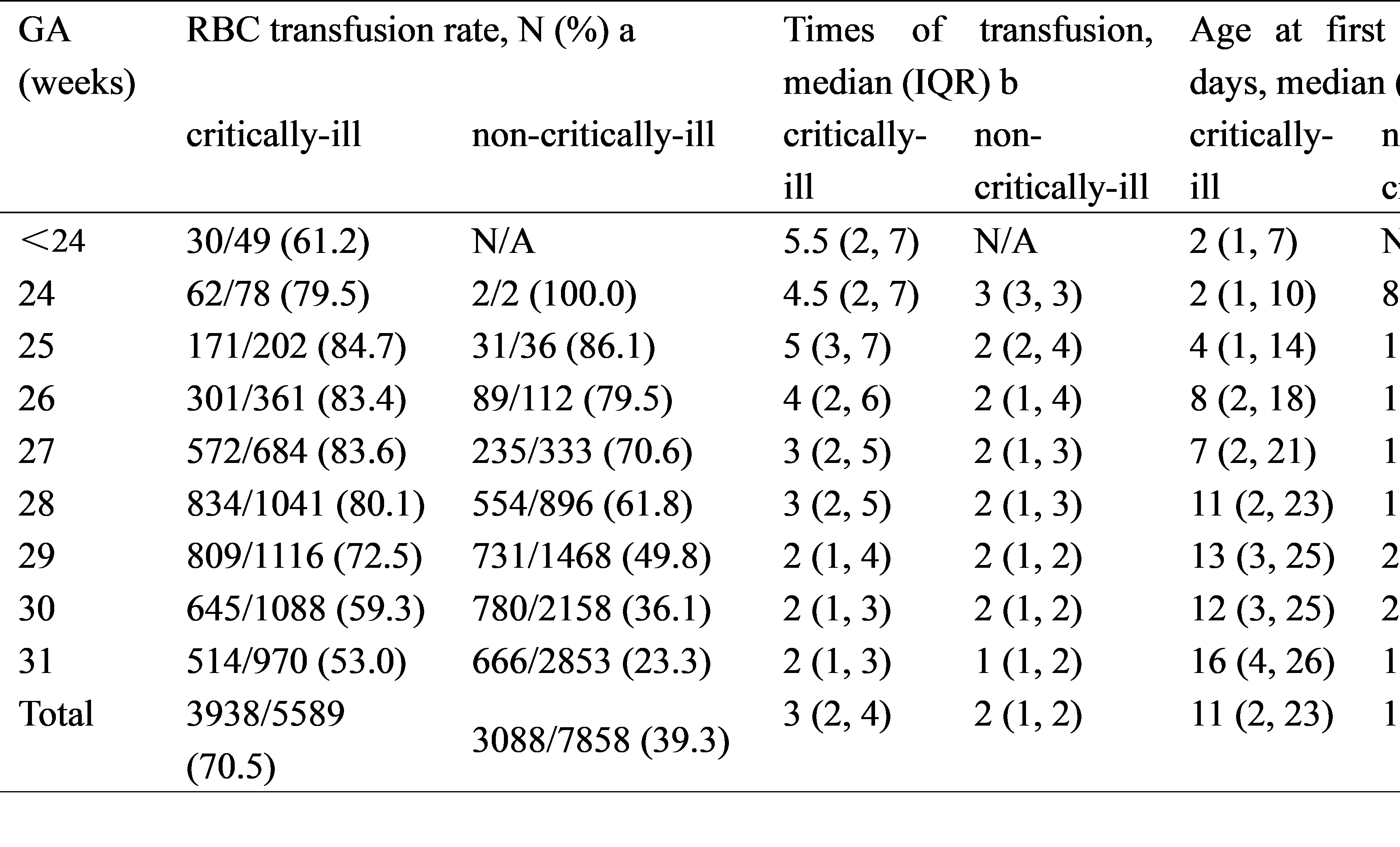
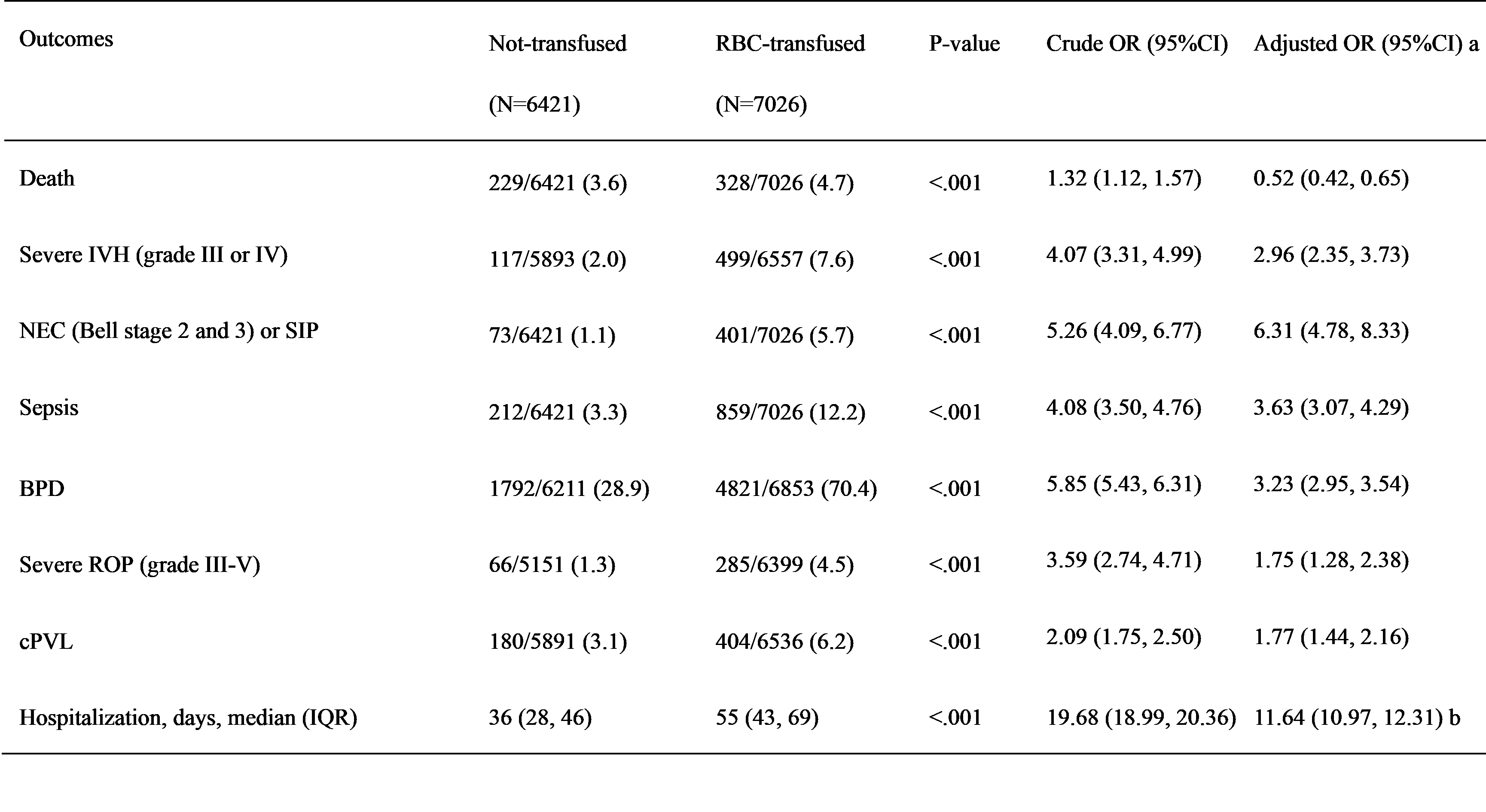
During the 2-years study, a total of 13,447 VPIs admitted to our NICUs were enrolled, of whom 7,026 (52.2%) received ≥1 RBC transfusions. The mean number of transfusions during hospitalization per infant was 2 (interquartile range, IQR 1 to 4 times) and the median age at first transfusion for all VPIs was 15 days (IQR 3-27 days). Even in the most mature VPIs born ≥29 weeks’ GA, there were still up to 42.9% (4145 of 9653) of infants received RBC transfusion. And in the subgroup, transfusion rate was higher in the critically ill group compared with infants in the non-critically ill group (70.5% vs 39.3%). The transfusion rate varied widely among different NICUs from 13.54% to 95%, and the variation remained significant after adjustment. Compared to the non-transfused group, the incidences of death, severe IVH, NEC or SIP, sepsis, BPD, severe ROP and cPVL, were significantly higher in the transfused group. After adjustment, the risk of all outcomes except death remained higher in the transfused group. In the subgroup of non-critically ill infants, RBC transfusion remained independently associated with BPD, severe ROP and cPVL.
Conclusion(s):
In this manuscript, our study for the first time provides baseline data on RBC transfusions in VPIs, showing an alarmingly high RBC transfusion rate among VPIs in China with significant site variations. There is an urgent need of national clinical practice guidelines to regulate the using of RBC products among VPIs.