Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 3: Gut Health Clinical Research
75 - Variation in management of patients with gastroschisis: Cross-sectional survey assessing perinatal and postnatal care in quaternary NICUs
Publication Number: 75.235
- AR
Ayan Rajgarhia, MD
Associate Professor of Pediatrics/ Attending Neonatologist
Children's Mercy Hospitals and Clinics
Kansas City, Missouri, United States
Presenting Author(s)
Background: Despite the relative frequency of gastroschisis, single centers often have insufficient volume to determine optimal care. Institutional and provider preference are difficult to separate from patient variability
Objective: To describe the spectrum of management for gastroschisis across level IV NICUs and identify opportunities for research, quality improvement, and consensus.
Design/Methods:
Cross-sectional survey in REDCap of Children’s Hospitals Neonatal Consortium (CHNC) (1 response per center) conducted June to October 2021 addressing antenatal, surgical, and neonatal care for patients with gastroschisis, including perinatal, delivery room, nutritional, and procedural management.
Results:
Response rate was 55% (22/40 sites); 95% neonatologists and 1 pediatric surgeon. Responding centers represented 77.2% of gastroschisis in the CHNC’s database in the 2 years preceding the survey.
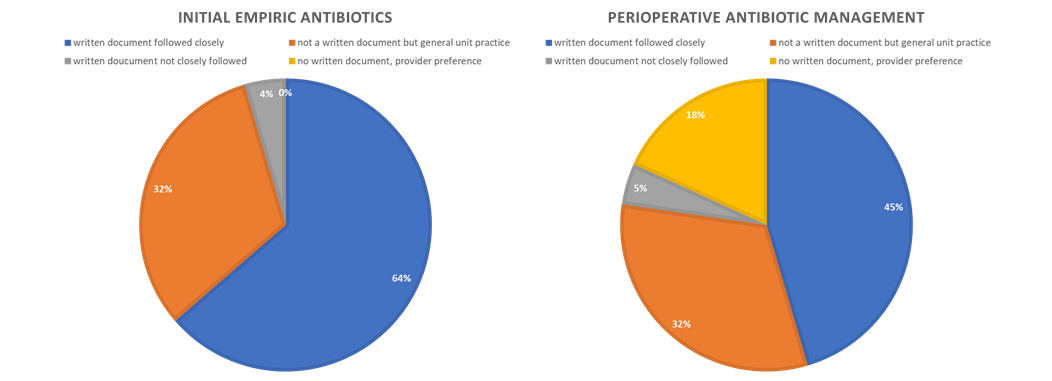
Recommended delivery ranged from 35 weeks to “term” (median 38 weeks). Thirteen NICUs (59%) reported starting empiric antibiotics on all patients. Use of perioperative antibiotics varied across centers, including dependence on initial empiric antibiotics, type of closure, and other bowel findings.
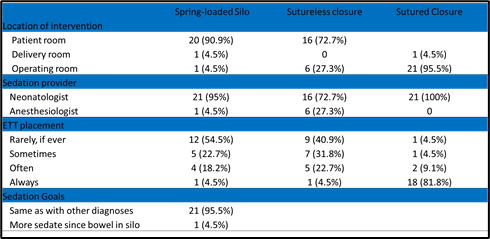
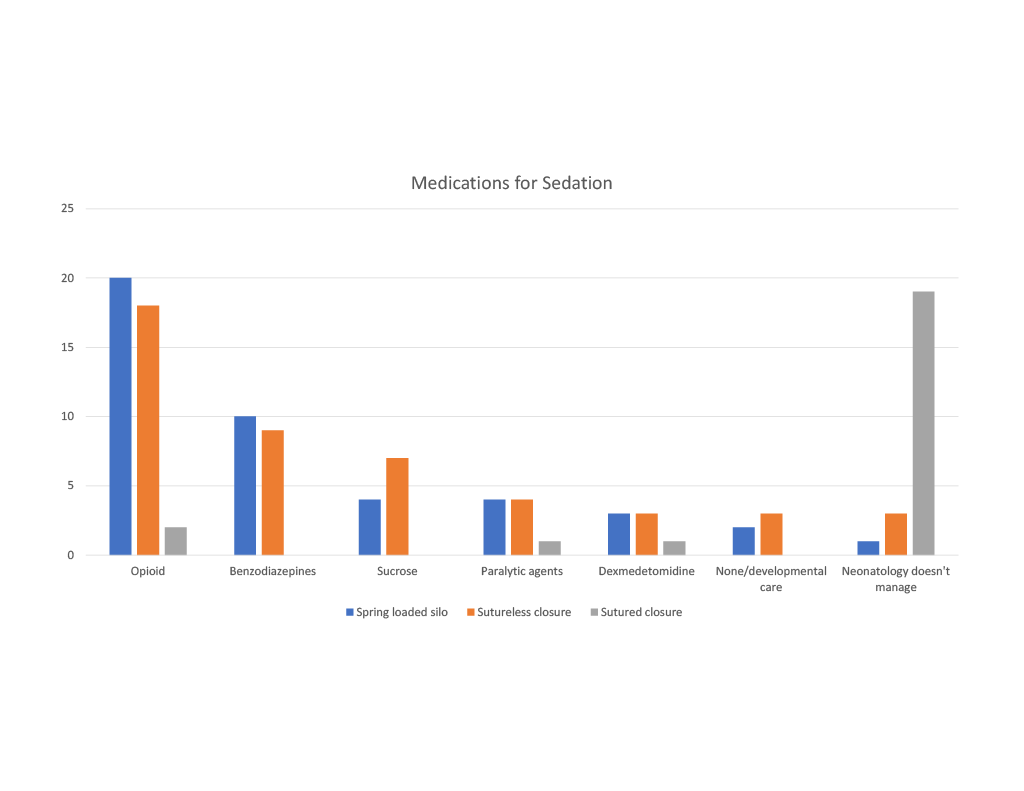
Institutional preference for closure timing (7/10 centers immediate vs. staged) and type (9/13 centers sutureless vs. sutured) varied from that occurring more often (delayed sutured). Spring-loaded silo placement and sutureless closure most often occurred at the NICU bedside with sedation by neonatologists and use of systemic opioids (20 & 18 centers, respectively) and benzodiazepines (10 & 9 centers, respectively). Sedation for sutured closure was mostly managed in the operating room by anesthesiology. Endotracheal intubation was reported to occur rarely/never at 12 centers (54.5%) for silo placement and 9 centers (40.9%) for sutureless closure. Most centers stated not having a formal limit of noninvasive respiratory support while in a silo or following closure.
Of 13 domains queried regarding institutional guidelines, a median of 7 centers/domain reported “written followed closely” and median 9 centers/domain “unwritten but consistent unit practice.” Most frequent written guidelines related to initial empiric antibiotics (68.1%) and feeding (68.1%), and most lacking were respiratory support (27.2%) and medications (22.7%).
Conclusion(s): Many level IV NICUs have guidelines or well-adopted practices for management of gastroschisis, but there is variation in availability of and adherence to these recommendations, and practice across centers. Identified areas for standardization include antibiotics, sedation, and respiratory support.