Neonatal-Perinatal Health Care Delivery: Practices and Procedures
Neonatal-Perinatal Health Care Delivery 3: Practices: Growth & Nutrition, Potpourri
769 - Pilot of Bilateral Infant Stimulation Study (BLISS) in the NICU
Publication Number: 769.247

Emily K. Garavatti, MD (she/her/hers)
Neurodevelopmental Disabilities Fellow
Oregon Health & Science University
Portland, Oregon, United States
Presenting Author(s)
Background:
Parents of infants admitted to the NICU often have clinically significant PTSD symptoms at time of discharge. Positive touch interventions have benefits for infants and parents, but current interventions cannot be implemented with critically ill infants. Therefore, our most at risk population is in need of interventions that use positive touch for both the parent and infant.
Objective:
We propose using a bilateral alternating stimulation technique as a form of positive touch for parents to engage with critically ill infants. We hypothesize this intervention will reduce infant autonomic arousal and reduce parental distress and anxiety. Our study aims to identify whether this intervention is feasible in the NICU setting and acceptable to parents and NICU staff, as a first step in intervention development.
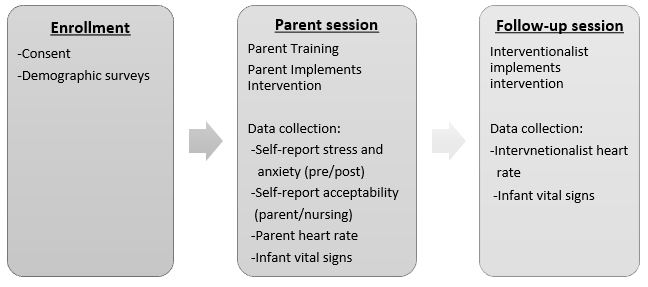
Design/Methods: This single arm feasibility and acceptability study was conducted in a level IV pod-based NICU. Parents were first instructed at bedside by an interventionist and then engaged their infant in the intervention. Outcomes included: parent heart rate (via wristband smartwatch); infant vital signs from bedside monitors; acceptability questionnaires; and parent self-report measures. See Figure 1.
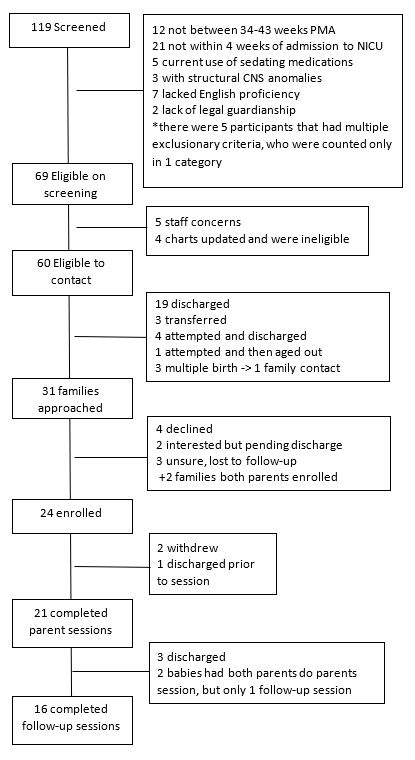
Results: We enrolled 24 parent-neonate dyads between June to September 2022. Twenty-one parents completed initial sessions (88%) and 16 infants completed follow-up sessions (76%). See Figure 2.
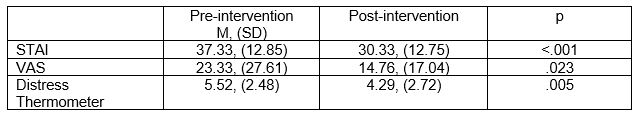
Feasibility benchmarks were met, with 100% of sessions completed without termination. Interventionists rated 81% of sessions positively, no sessions were rated negatively. Parents wore wristbands for 100% of sessions. Infant vital signs were collected for 76% of sessions. High levels of acceptability were reported, with a mean score on Client Satisfaction Questionnaire (CSQ-8) of 30.84 (score range 8-32) for parents and mean score on Acceptability of Intervention Measure (AIM) of 34.77 (score range 8-40) for nursing staff. State anxiety was measured using the Visual Analog Scale- Anxiety (VAS-A) and the State Trait Anxiety Inventory (STAI), and psychological distress was measured using the Distress Thermometer. Although the feasibility study was not powered to determine effects; preliminary findings indicate potential for the intervention to decrease anxiety and psychological distress in parents post-intervention. See Table 1.
Conclusion(s):
The BLISS study is feasible to conduct in a pod-based NICU and is acceptable to both parents and nursing staff. Preliminary data suggests the intervention is promising for further pursuit on the impact on parental anxiety and distress.