Breastfeeding/Human Milk
Breastfeeding/Human Milk 4: Breastfeeding and Milk Provision
30 - Infant milk intake in the first 24 hours of life: How much is too much?
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 30
Publication Number: 30.202
Publication Number: 30.202
Igbagbosanmi O. Oredein, Michigan State University College of Human Medicine, Grand Blanc, MI, United States; Mohammed Al-Nahar, Michigan State University College of Human Medicine, Grand Blanc, MI, United States; Nathalee Harris, Hurley Medical Center, Montrose, MI, United States; Navin Kumar, Michigan State University College of Human Medicine, Grand Blanc, MI, United States

Igbagbosanmi O. Oredein, MD, MPH (she/her/hers)
Chief Resident
Michigan State University College of Human Medicine
Grand Blanc, Michigan, United States
Presenting Author(s)
Background: Volumes of formula supplementation in breastfed infants and exclusive formula feeds in the first 24 hours of life (HOL), often does not match the estimated physiological newborn stomach capacity. How this affects early feeding intolerance (FI), especially in relation to birth weight (BW) and gestational age (GA), is not well quantified.
Objective: To assess the impact of the volume of milk intake per kg BW on neonatal FI in the first 24 HOL, among late preterm (LPT) and term infants.
Design/Methods: Single-center retrospective chart review of 6650 infants born from March 2018 to March 2021 at GA ≥ 35 weeks and admitted to the newborn nursery after birth. Volumes of each formula feed per kg BW, in the first 24 HOL, were assessed. FI was defined as chart documentation of emesis, abdominal distension, need for an abdominal x-ray, and/or switch to a sensitive formula. Overall feeding volumes were first correlated with GA and FI. Subsequently, multiple logistic regression analyses correcting for confounding variables (maternal race, age, parity, marital status, mode of delivery, use of anesthesia at delivery, maternal insurance and co morbidities: diabetes, hypertension, anemia, illicit drug use, psychiatric illness, as well as neonatal prematurity and BW) were performed to analyze the odds of neonatal FI with increasing feeding volumes. Results are reported as adjusted OR (95% CI).
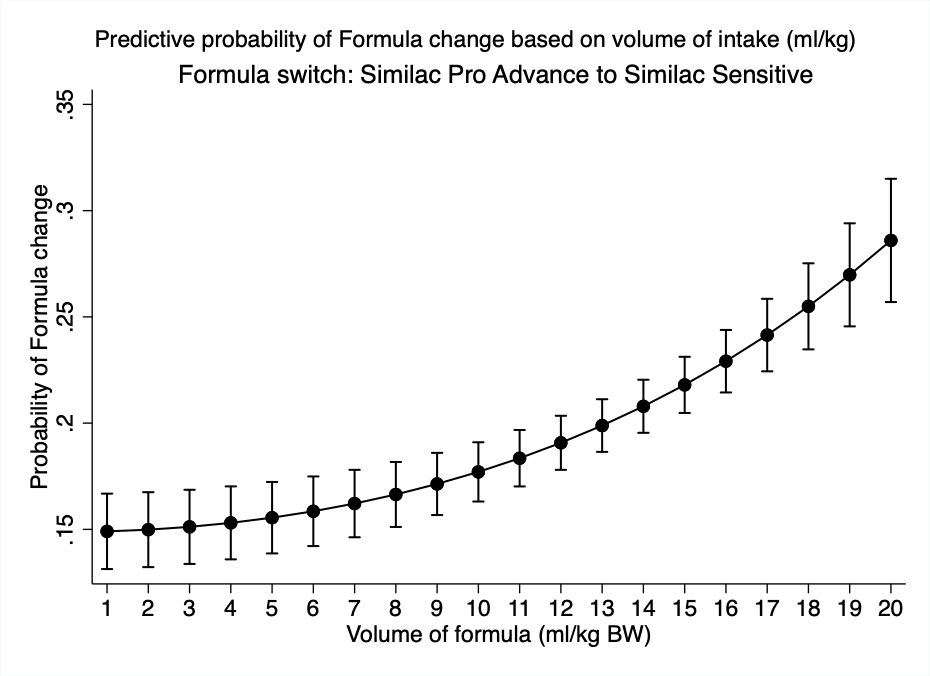
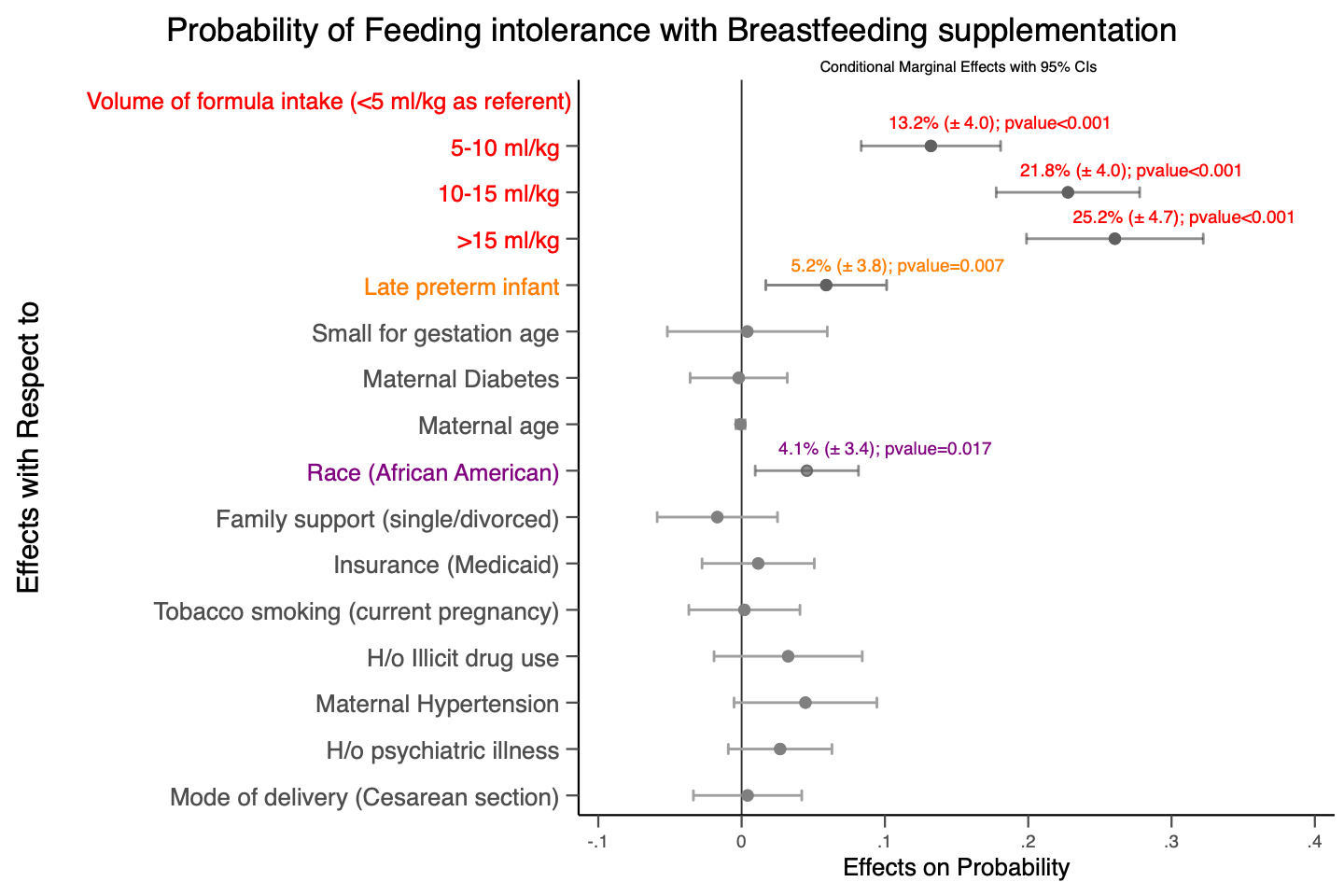
Results: Of the total 6650 infants, 21.9% (n = 1456) were exclusively breastfed, 46.6% (n = 3102) were supplemented with formula and 31.5% (n = 2092) were exclusively formula fed. The maximum volume of formula intake per feed was inversely correlated with GA and was higher with FI vs no FI (β = -1.39 vs -1.28, p < 0.001). There were 2.5 (1.4 - 4.6) times higher odds of emesis in LPT infants with first feeding volume > 8 ml/kg [Model 1], and 2.2 (1.8 - 2.6) times higher odds of formula switching in exclusively formula fed infants with volumes > 10.5 ml/kg [Model 2]. Among breastfed infants supplemented with formula, compared to lower volumes of < 5 ml/kg, odds of overall FI increased by 2.8 (1.9 - 4.3)-, 4.6 (1.3 - 6.8)-, and 5.2 (3.4 - 7.9)- fold with 5 - 10, 10 - 15, and > 15 ml/kg of formula, respectively [Model 3]. Post estimation probability was calculated for all the 3 models [Figures 1-3].
Conclusion(s): Higher volumes of milk intake in relation to BW, often exceeds physiological newborn stomach capacity and is associated with early FI. Optimizing feeding volumes accounting for BW and GA may decrease a good proportion of early FI in neonates as they may, in reality, be experiencing a volume intolerance issue.
.jpg)