Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 3: Gut Health Clinical Research
66 - Risk Factors and Epidemiology of Spontaneous Intestinal Perforation Among Infants Born at 22-24 Weeks Gestational Age
Publication Number: 66.235

Ryan Kilpatrick, MD (he/him/his)
Fellow
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background:
Infants born at 22-24 weeks gestational age (GA) are at increased risk of spontaneous intestinal perforation (SIP). With increased resuscitation and survival among 22-24 week GA infants, more information is needed regarding the risk factors and epidemiology of SIP in this population.
Objective:
Describe the epidemiology, risk factors, and timing of SIP among infants born 22-24 weeks GA.
Design/Methods:
We conducted a multicenter observational cohort study of infants born 22-24 weeks GA admitted to a Pediatrix Medical Group neonatal intensive care unit from 2010-20. Infants with known congenital anomalies, bowel obstruction, cystic fibrosis, intestinal atresia, no recorded body weights by postnatal day 7, or death prior to postnatal day 2 were excluded. We used multivariable logistic regression to separately evaluate antenatal and postnatal factors associated with SIP. The antenatal model included all SIP occurrences. The postnatal model used medication exposures occurring within the first 3 postnatal days and SIP occurring postnatal day 3-14 to ensure that exposure occurred prior to SIP. All antenatal factors were included as covariates in the postnatal model. We used Pearson’s chi-square test to assess trends in SIP incidence by year. Results were reported as adjusted odds ratios (OR) with 95% confidence intervals (95% CI). Maximum weight loss was calculated as the lowest daily weight as a percentage of birth weight.
Results:
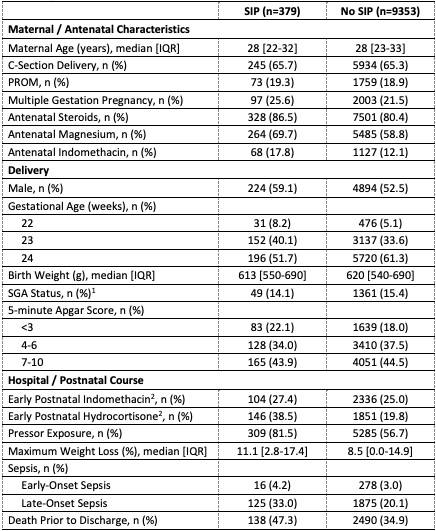
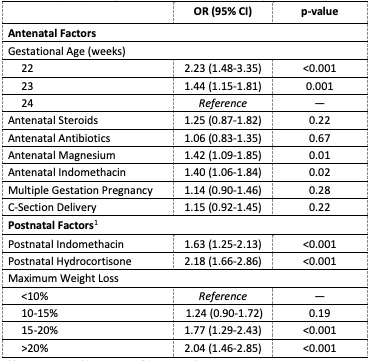
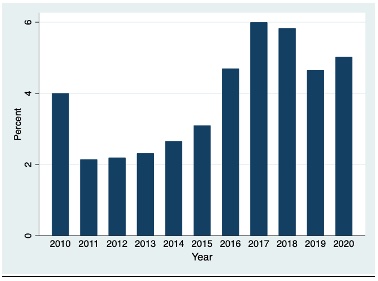
Of the 9712 22-24 week GA infants included, 379 (3.9%) developed SIP (Table 1). SIP incidence increased during the study period (p< 0.001) (Figure 1). The median time from birth to SIP was 7 days (Q1, Q3: 5, 10). Compared to infants born at 24 weeks GA, the odds of SIP were higher for infants born at 22 weeks GA (OR 2.23 (95% CI 1.48-3.35)) and 23 weeks GA (OR 1.44 (95% CI 1.15-1.81)) (Table 2). Antenatal factors associated with SIP included magnesium exposure (OR 1.42 (95% CI 1.09-1.85)) and indomethacin exposure (OR 1.40 (95% CI 1.06-1.84)). Postnatal factors associated with SIP included exposure to indomethacin (OR 1.63 (95% CI 1.25-2.13)) and exposure to hydrocortisone (OR 2.18 (95% CI 1.66-2.86)). Compared to infants with maximum weight loss of < 10% birth weight, infants who lost 15-20% (OR 1.77 (95% CI 1.29-2.43)) and >20% of birth weight (OR 2.04 (95% CI 1.46-2.85)) had higher odds of SIP.
Conclusion(s):
In this cohort of 22–24 week GA infants, antenatal exposure to magnesium or indomethacin, postnatal exposure to hydrocortisone or indomethacin, and weight loss >15% were associated with SIP.