Health Services Research
HSR 2: Clinical Explorations, Associations, and Interventions
598 - Evaluating the Implementation of Pediatric Inpatient Social Needs Screening in a Community Hospital
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 598
Publication Number: 598.223
Publication Number: 598.223
Jana C. Leary, Tufts Medical Center, Waban, MA, United States; Hannah R. Bagley, Floating Hospital for Children at Tufts Medical Center, Townsend, MA, United States; Jennifer L. Coates, Tufts University School of Medicine, Hudson, NH, United States; Arvin Garg, UMass Chan Medical School/UMass Memorial Health, Worcester, MA, United States; Karen Freund, Tufts University School of Medicine/ Tufts Medical Center, Boston, MA, United States
Jana C. Leary, MD, MS (she/her/hers)
Assistant Clinical Professor of Pediatrics
Tufts Medical Center
Waban, Massachusetts, United States
Presenting Author(s)
Background: Professional guidelines from the AAP recommend social needs screening at all child health visits, and CMS announced that inpatient social needs screening will become mandatory quality reporting by 2024. To date, no studies have evaluated screening in a community hospital. In April 2022, one local community hospital piloted the integration of a standardized social needs screening tool into routine pediatric admission intake.
Objective: Evaluate the impact of social needs screening tool implementation in a pediatric inpatient community hospital setting.
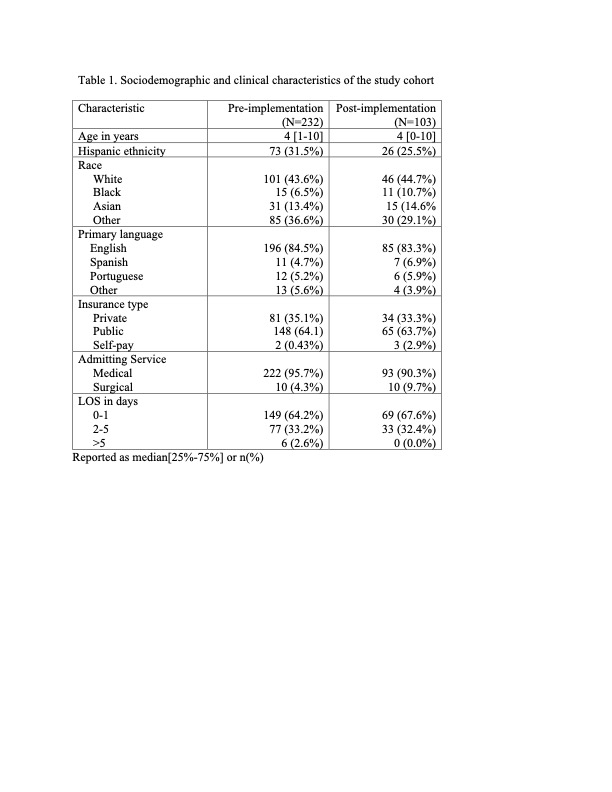
Design/Methods: Sociodemographic and clinical characteristics were extracted from the EHR for patients aged 0-18 years admitted to the pediatric unit at one community hospital between April 2021 (one year pre-implementation) and Sept 2022 (five months post-implementation). For a random subset of 232 pre-implementation (“pre-“) and 103 post-implementation (“post-“) patients, we performed manual data extraction, documenting any standardized questions asked about social needs and needs identified for 8 social domains, SW consults completed, time to SW consults, community resource referrals, and communication of social risks in discharge summaries. Given the pilot nature, not powered for statistically significant comparisons, we used descriptive statistics to compare outcomes between the pre- and post- groups.
Results: Sociodemographic characteristics were similar between the groups (Table 1). Screening rates were higher in the post-group for all domains except safety, and no pre- patients had comprehensive screening for 5+ domains (Table 2). The post- group had higher rates of social needs identified compared with the pre- group, for any needs: 17.8% v. 8.2%, and for each social domain except education. Social service consults were completed more frequently and earlier for the post- group compared with pre- group, 11.8% v. 5.6%, and median 21hrs v. 25hrs, respectively. Community resource referral rates and frequency of social risks documented in discharge summaries were higher in the post- group compared with pre- group, 4.9% v. 3.9%, and 19.6% v. 8.6%, respectively.
Conclusion(s): At one community hospital, implementation of a standardized social needs screening tool increased needs identified in nearly all screened domains, and increased social service consultations, community resource referrals, and written communication of social risk in discharge summaries. Future work will include improvement efforts to increase resource referrals, and mixed methods research to assess feasibility and acceptability of sustained screening in community hospital settings.
.jpg)
