Health Services Research
HSR 2: Clinical Explorations, Associations, and Interventions
596 - Factors in early diagnosis and treatment of infants with atypical motor development: family experience and the role of social influencers of health
Publication Number: 596.223

Nina L. Alfieri, MD MS (she/her/hers)
Attending Physician, Instructor of Pediatrics
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background:
Little is known about caregivers’ experiences regarding their child receiving a diagnosis of atypical motor development and accessing treatment. Examining the role of social influencers of health (SIOH) on health care access and outcomes can inform opportunities for system change and improve access to resources for infants with motor delay.
Objective:
To understand the process of diagnosing and treating atypical motor development through a caregiver lens and to explore the role of SIOH in accessing therapy.
Design/Methods:
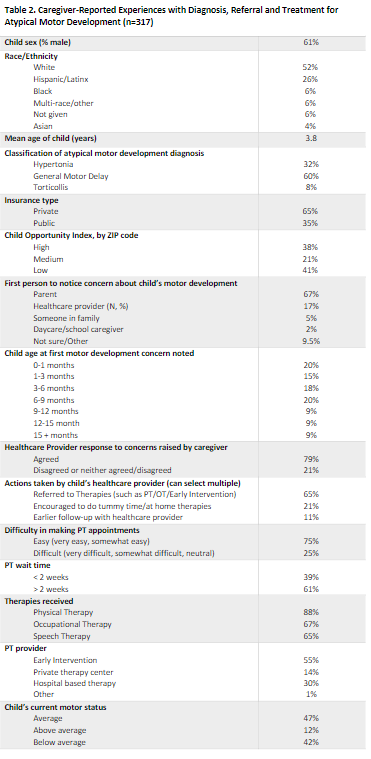
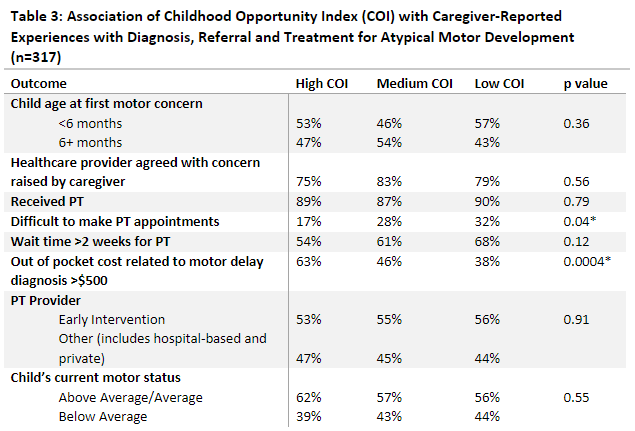
Cross-sectional survey of caregivers of children 0-3 years old with a diagnosis of atypical motor development seen at Lurie Children’s Hospital between 2017-2021. Participants were invited to take an SMS/email Qualtrics survey designed by the authors over 2 weeks in December 2022; a $10 gift card was offered as incentive. Survey items related to the process of receiving the child’s diagnosis, referrals and receipt of therapy, primary care provider guidance, and costs of care. Responses were linked with the child’s electronic medical record. ZIP code-level estimates of Child Opportunity Index (COI) were used to examine associations between neighborhood opportunity and health outcomes. A bivariate logistic regression was performed to examine the relationship of COI with difficulty in making PT appointments.
Results:
Of the 4473 caregivers of patients with an atypical motor diagnosis invited to complete the survey, 831 initiated (19% response rate), 715 completed (86% completion rate). After excluding 121 due to missing EMR data, 317/588 (54%) caregivers responded that their child had a motor delay diagnosis and comprised the final sample. Concerns about motor development were first noticed by 6 months of age in 53% of children and by 9 months in 73%. Most often caregivers were first to notice a motor delay (67%), followed by the child’s healthcare provider (17%). When caregivers raised concerns to the child’s provider, 78% of providers agreed and 65% of patients were referred to therapies. Making PT appointments was rated as “difficult” by 25% of families; 61% waited >2 weeks for initial PT, and 50% paid >$500 out of pocket for PT. Compared with children living in ZIP codes with high COI, those with lower COI had 2.3x higher odds of difficulty making PT appointments (95% CI 1.2-4.3). There was no difference in wait time for PT or receipt of PT based on COI.
Conclusion(s):
Caregivers recognize atypical motor delay in early infancy and providers often agree with these concerns and refer for therapy. PT access is a challenge, especially for children with lower neighborhood opportunity..png)