Health Services Research
HSR 2: Clinical Explorations, Associations, and Interventions
595 - Trends in Respiratory Syncytial Virus Seasonality and Timing of Immunoprophylaxis Administration
Publication Number: 595.223

Jennifer Kusma, MD, MS (she/her/hers)
Attending
Ann & Robert H. Lurie Children's Hospital of Chicago
Ann & Robert H Lurie Children’s Hospital/ Northwestern University
CHICAGO, Illinois, United States
Presenting Author(s)
Background:
High-risk children are eligible for RSV immunoprophylaxis (RSV-IP) per American Academy of Pediatrics (AAP) guidelines. RSV-IP is typically made available by insurers in the US annually from November to March, correlating with previously observed RSV seasonality. However, the extent to which RSV-IP policy decisions have left high-risk children unprotected outside of the typical RSV season has not been studied.
Objective:
To evaluate trends in the timing of RSV hospitalizations across the United States over the past five years and examine disruptions in RSV seasonality as a result of the COVID-19 pandemic.
Design/Methods:
We performed a retrospective cross-sectional analysis of RSV hospitalizations from July 1, 2017- June 30, 2022, including children < 2 years. We used diagnosis codes to identify high-risk infants and RSV hospitalizations. We characterized the timing of RSV seasonal spikes and compared RSV seasonality to the availability of RSV-IP based on guideline timing.
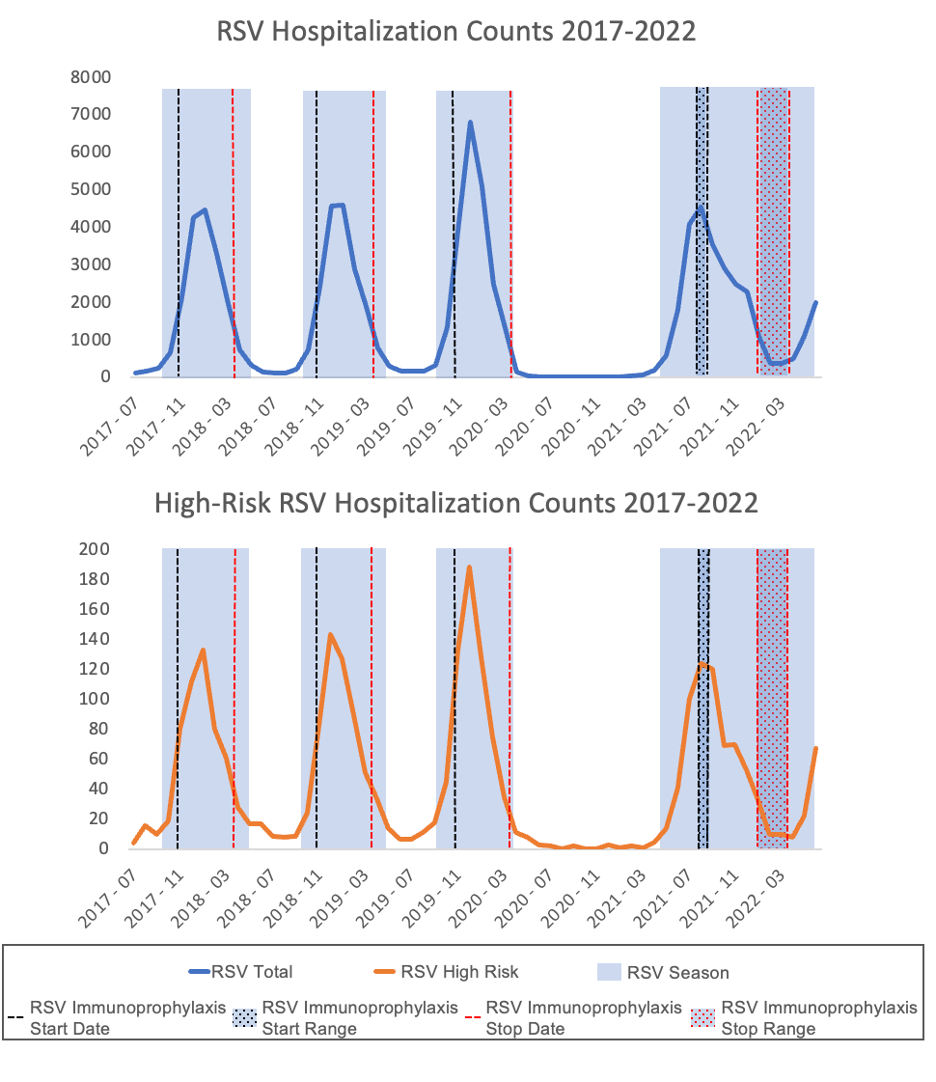
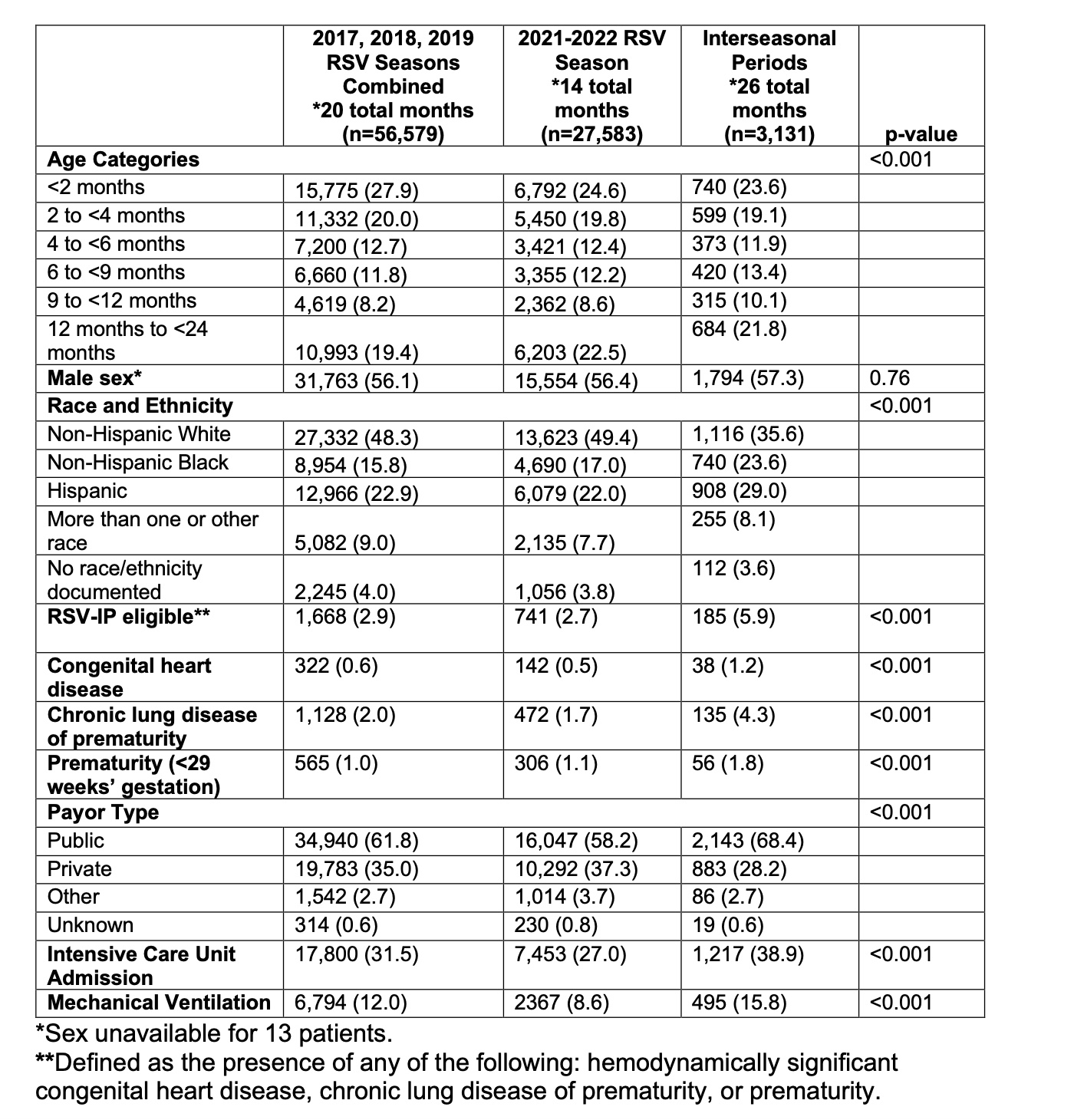
Results: We identified four RSV seasonal spikes over the past five years, with seasonal spikes in 2017-2019 following the typical seasonal pattern beginning in October (Figure). In 2021, the seasonal spike began in May. Updated guidance for RSV-IP was not published until August 2021 and was subsequently approved by most payors in the following weeks. As a result, there were months when RSV was circulating in communities and high-risk children were left unprotected. We found that while there were fewer RSV hospitalizations during the time between seasons, high-risk children made up a larger proportion of those hospitalized (Table). During the RSV interseason, there were a greater proportion of admissions requiring mechanical-ventilation and to intensive care settings.
Conclusion(s): Shifting RSV epidemiology requires flexible policy decisions about timing of RSV-IP. Guidance based on historic seasonality does not align with current national trends of RSV hospitalization incidence, leaving high-risk children unprotected and at risk for RSV. Flexible policy informed by real-time epidemiology is critical to ensure adequate RSV prevention for high-risk children when RSV is circulating.