Health Services Research
HSR 1: States, Medicaid, and the Structure of Health Care
574 - Driving Investment in Pediatric Alternative Payment Models: Lessons from the North Carolina Integrated Care for Kids Model
Publication Number: 574.222
.jpg)
Greeshma James, MPH (she/her/hers)
Policy Analyst
Duke University School of Medicine
Durham, North Carolina, United States- RC
Rushina Cholera, MD PhD (she/her/hers)
Assistant Professor of Pediatrics and Population Health Sciences
Duke University School of Medicine and Duke Margolis Center for Health Policy
Durham, North Carolina, United States
Presenting Author(s)
Background:
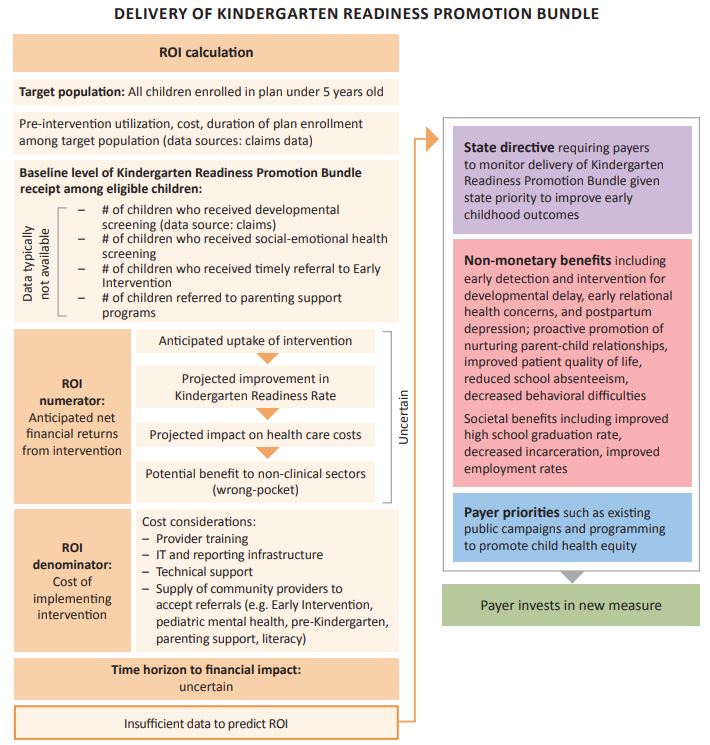
Alternative payment models (APMs) reward efficient and effective care rather than volume of care. Given the unique health and social needs of children, pediatric APMs face difficulty demonstrating return on investment (ROI) as payers typically prioritize short-term ROI. The Centers for Medicare and Medicaid Services’ Integrated Care for Kids (InCK) model is a pilot for Medicaid-enrolled children that promotes pediatric APM innovation. North Carolina InCK (NC InCK) developed a pediatric APM that includes traditional performance measures and cross-sector measures on kindergarten readiness and social needs.
Objective:
To use the NC InCK pediatric APM experience to describe how ROI for pediatric measures can be considered in APM design and implementation.
Design/Methods:
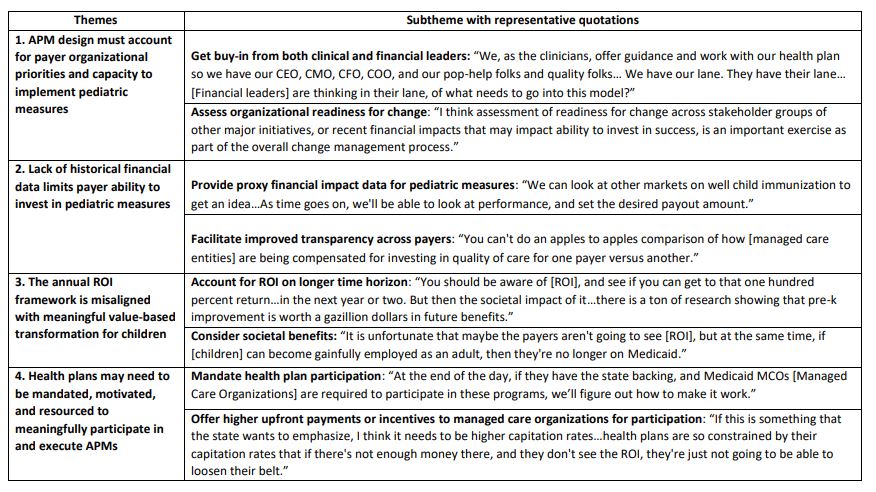
We conducted interviews with national healthcare actuaries (n=4) and NC health and policy experts (n=5) who participated in the NC InCK APM design. Interviews focused on understanding how pediatric APM measures are conceptualized and identifying generalizable strategies for pediatric APM implementation given ROI considerations. Rapid qualitative analysis was used to identify major themes.
Results:
Interviews revealed four themes (Table 1): 1) APM design should account for payer organizational priorities and capacity to implement new measures. Both clinical and financial leaders at payer organizations should be aligned on new pediatric measures and their financial feasibility. 2) Novel cross-sector pediatric measures (e.g. K-readiness, food) often lack historical performance data, limiting payer investment. Providing payers with data for financial and operational resources required to implement new measures can address this barrier (Figure 1). 3) The ROI framework is inadequate for driving investment in pediatric metrics, which often focus on children’s long-term health and may take years to demonstrate an ROI. Getting buy-in from payers on the non-financial value of novel measures like k-readiness and bundling them with accepted, existing metrics could help. 4) Mandates can encourage health plans to invest in and execute pediatric APMs. Additional payments for meeting performance metrics or withholding of funds for underperformance may be necessary to motivate investment.
Conclusion(s):
Value-based transformation through pediatric APMs necessitates a shift away from the ROI framework focused on financial returns to achieve meaningful investment in children’s health and social needs. Actionable strategies recommended by APM strategic and operational experts are identified to facilitate broader adoption of pediatric APMs.