Health Services Research
HSR 2: Clinical Explorations, Associations, and Interventions
586 - Parent (caregiver) Reported Outcomes of COVID-19 after at least 90 days
Publication Number: 586.223

Lawrence C. Kleinman, MD, MPH, FAAP (he/him/his)
Professor, Vice Chair, Director
Rutgers, Robert Wood Johnson Medical School
New Brunswick, New Jersey, United States
Presenting Author(s)
Background:
Post-acute sequelae of COVID-19 (PASC) in children occur and include an ill-defined entity known as “long COVID”. We took advantage of an ongoing NIH-funded study of acute COVID-19 to gain insight into caregiver (parent) perspectives regarding children and adolescent’s experiences of long COVID and symptoms.
Objective: Describe parent-reported outcomes of children who experienced COVID-19, drawn from each of 3 cohorts defined by their early COVID-19 experience (1. mild/asymptomatic, 2. pneumonia/acute respiratory distress syndrome; and 3. Multisystem Inflammatory Syndrome in Children (MIS-C)).
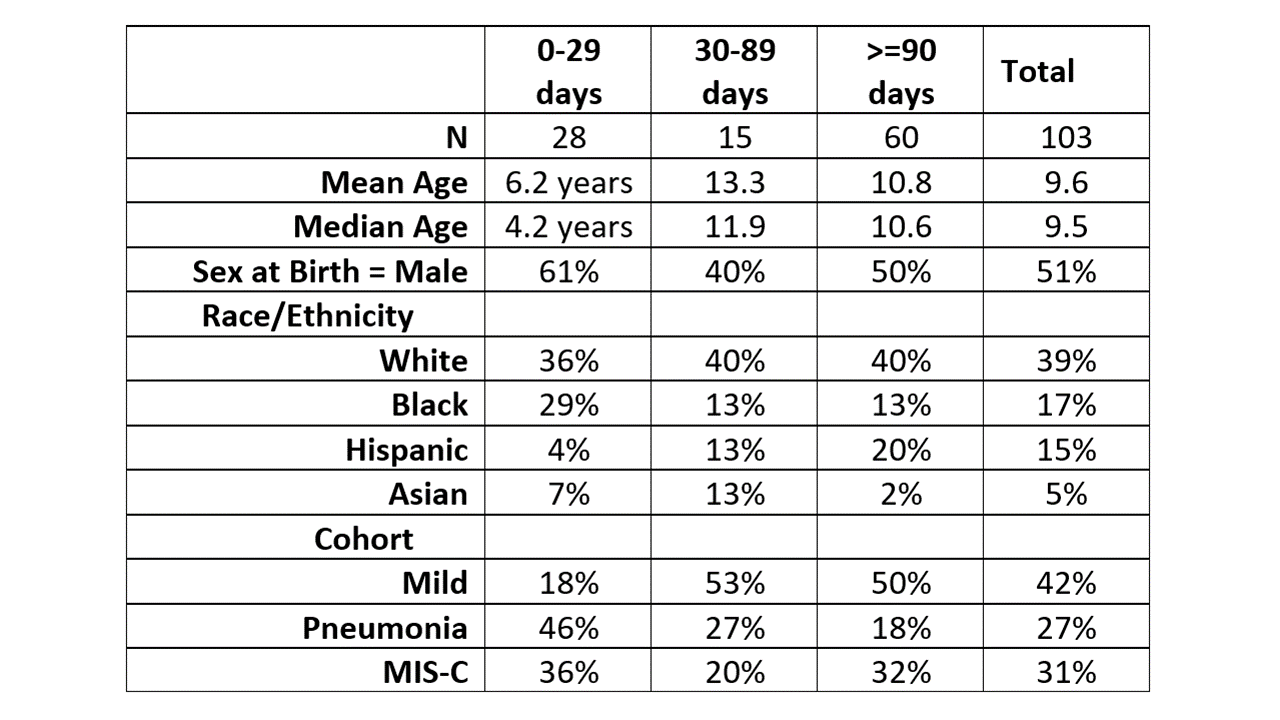
Design/Methods: The Rutgers CONNECT study collected caregiver-reported findings from the cohorts of children/adolescents who experienced COVID-19, described in the Objectives. Some children were enrolled around the time of infection and others after convalescence. 60 of 103 were surveyed at least 90 days post-infection.
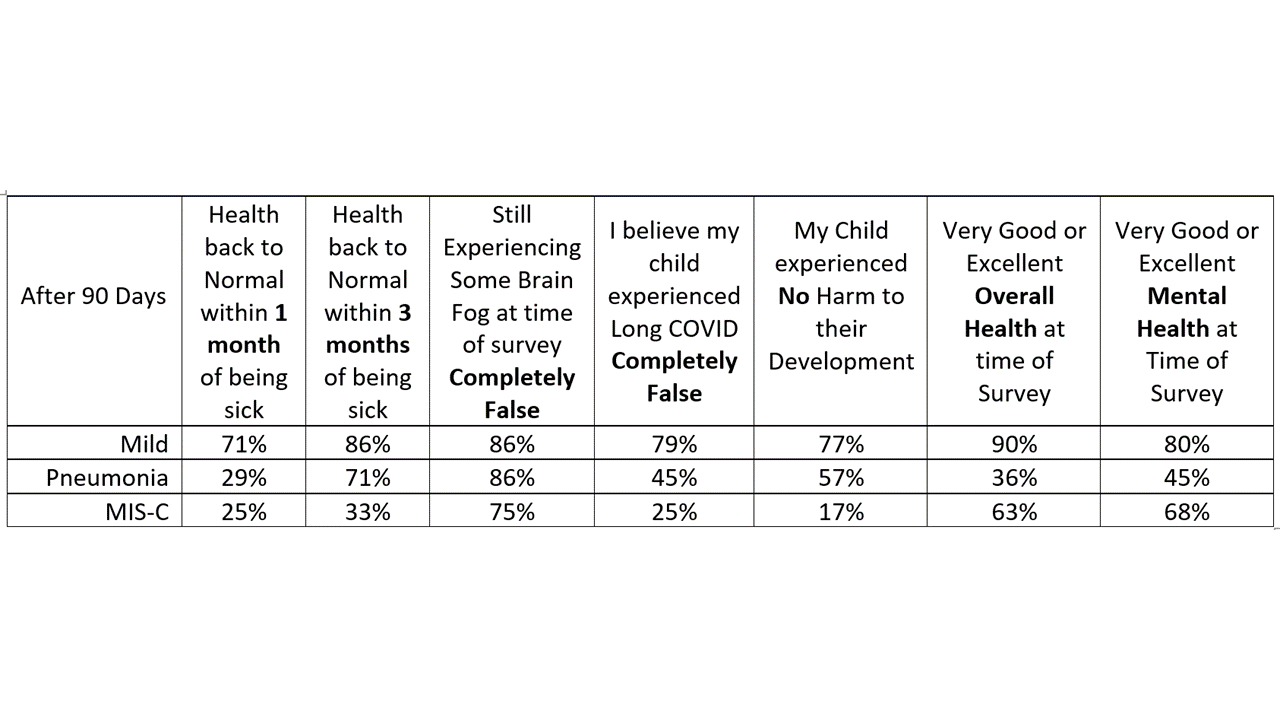
We used a Survey based upon the validated LINK answer set, developed and used at Rainbow Babies and Children’s Hospital for the past 5 years. The 5-point Likert scale ranges from Completely False to Completely True and is dichotomized at each extreme, depending on the wording of the stem. It is completely true that the respondent sees the child as back to their baseline health, or it is not. A parent reports is as completely false that as the children is experiencing brain fog or they do not. Similarly a parent describes as Completely False that they think their child had Long COVID or they do not.
Results:
Characteristics of our sample are shown in Table 1. Key parent-reported measures for those who were surveyed 90 days or more after their initial illness are summarized in Table 2.
Conclusion(s):
Using CDC definitions of long COVID defined as symptoms after 30 days, parents in each cohort reported high rates of symptoms at 1 month with meaningful proportions continuing symptoms at 3 months (consistent with the WHO definition of long COVID). Parent-reported perspectives on whether their child had long COVID track in between the 1 and 3 month measures. Large proportions of parents, especially in the MIS-C population perceive harm to their child’s development.
While our sample size is modest, we present evidence of substantial proportions of children who have caregiver-reported findings that are consistent with long COVID. Even after 90 days or more, Pneumonia and MIS-C patients are less likely to have their health reported as very good or excellent than those who had more mild disease. Parent-reports contribute to understanding child health outcomes of COVID-19.