Infectious Diseases
Infectious Diseases 2
629 - A Geospatial Analysis of Community-Acquired Extended-Spectrum Beta-Lactamase Urinary Tract Infections in Children Living in the Washington Metropolitan Area
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 629
Publication Number: 629.226
Publication Number: 629.226
Yifeng Wang, The George Washington University, Washington, DC, United States; Maria S. Rueda Altez, Children's National Health System, Washington, DC, United States; Maria C. Ortiz Vergara, Childrens national hospital, Gaithersburg, MD, United States; Rana F. Hamdy, Children's National Hospital, Washington, DC, United States; Anand Gourishankar, Children's National Health System, Washington, DC, United States

Yifeng Wang, B.S. (he/him/his)
Medical Student
The George Washington University
Washington, District of Columbia, United States
Presenting Author(s)
Background: The incidence of community-acquired extended-spectrum beta-lactamase (ESBL) urinary tract infections (UTI) is rising, and they are associated with adverse patient outcomes and increased healthcare costs. Several clinical risk factors for ESBL UTI have been identified. However, more information is needed about how geographic and social factors affect ESBL UTI and its distribution. The CDC Social Vulnerability Index (SVI) is a composite measure of social risk factors on human health at the community level, and its relationship with UTI is unknown.
Objective: To identify the distribution and geographic hot spots for ESBL UTI in children from the DC metropolitan area and compare the distribution of the SVI for cases with ESBL UTI.
Design/Methods: A retrospective case-control study was conducted among children 1 month to 18 years of age diagnosed with UTI at an emergency department from January 2019 to December 2021. Our definition for UTI included a positive urine culture ( >=10^5 CFU for clean catch, >=5x10^4 for catheterized, and >0 for suprapubic puncture samples), abnormal urinalysis (positive leukocyte esterase and/or >=10 WBC), and symptoms consistent with urinary tract infection. We randomly selected matched cases (ESBL UTI) to controls (non-ESBL UTI) by age and gender in a 1:3 ratio. Cases with recent (< 3 months) hospitalization or long-term care facility stay were excluded from the study. The hotspot and SVI maps were created with ArcGIS Pro. Conditional logistic regression was used for the association between SVI and UTI.
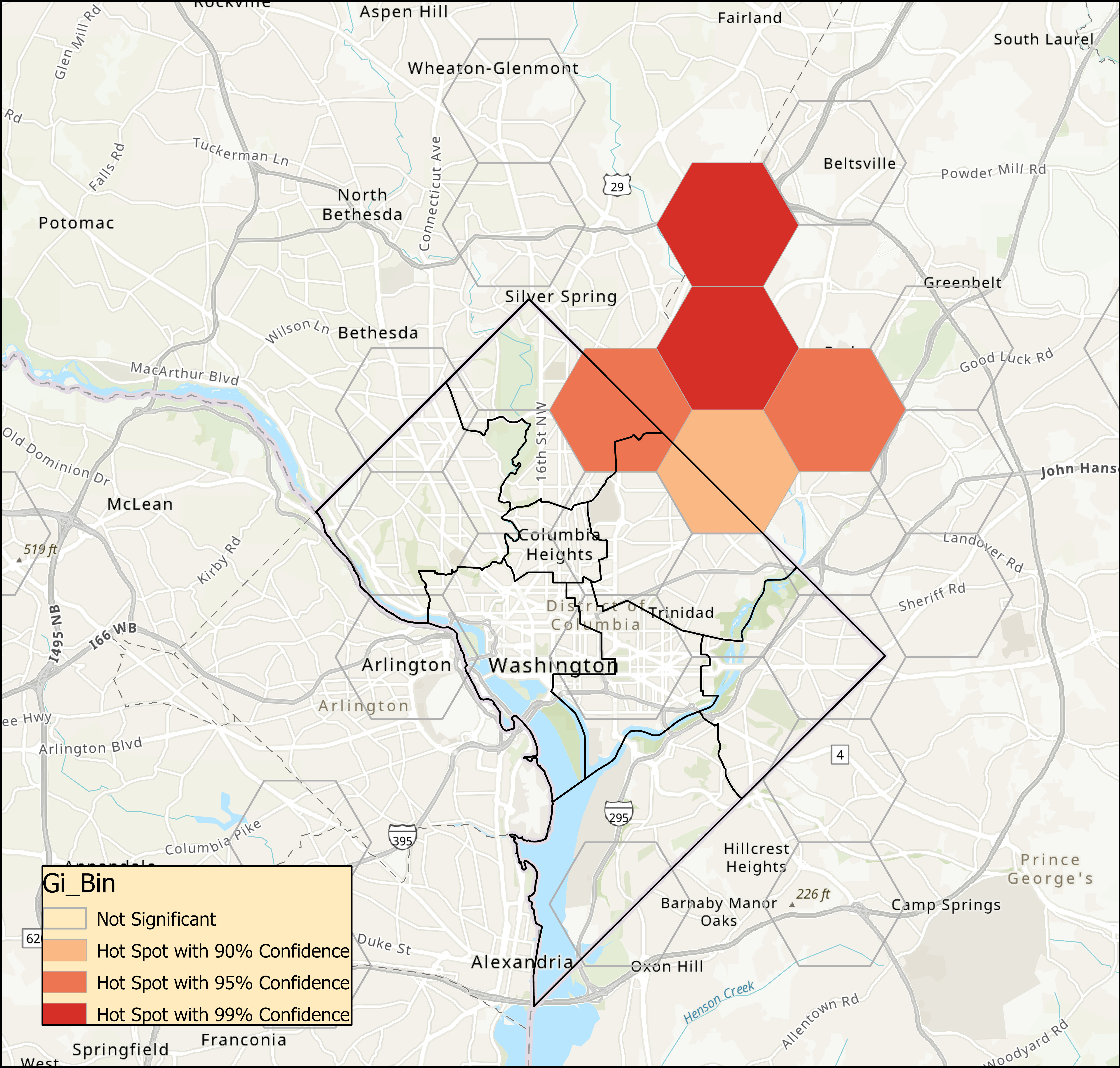
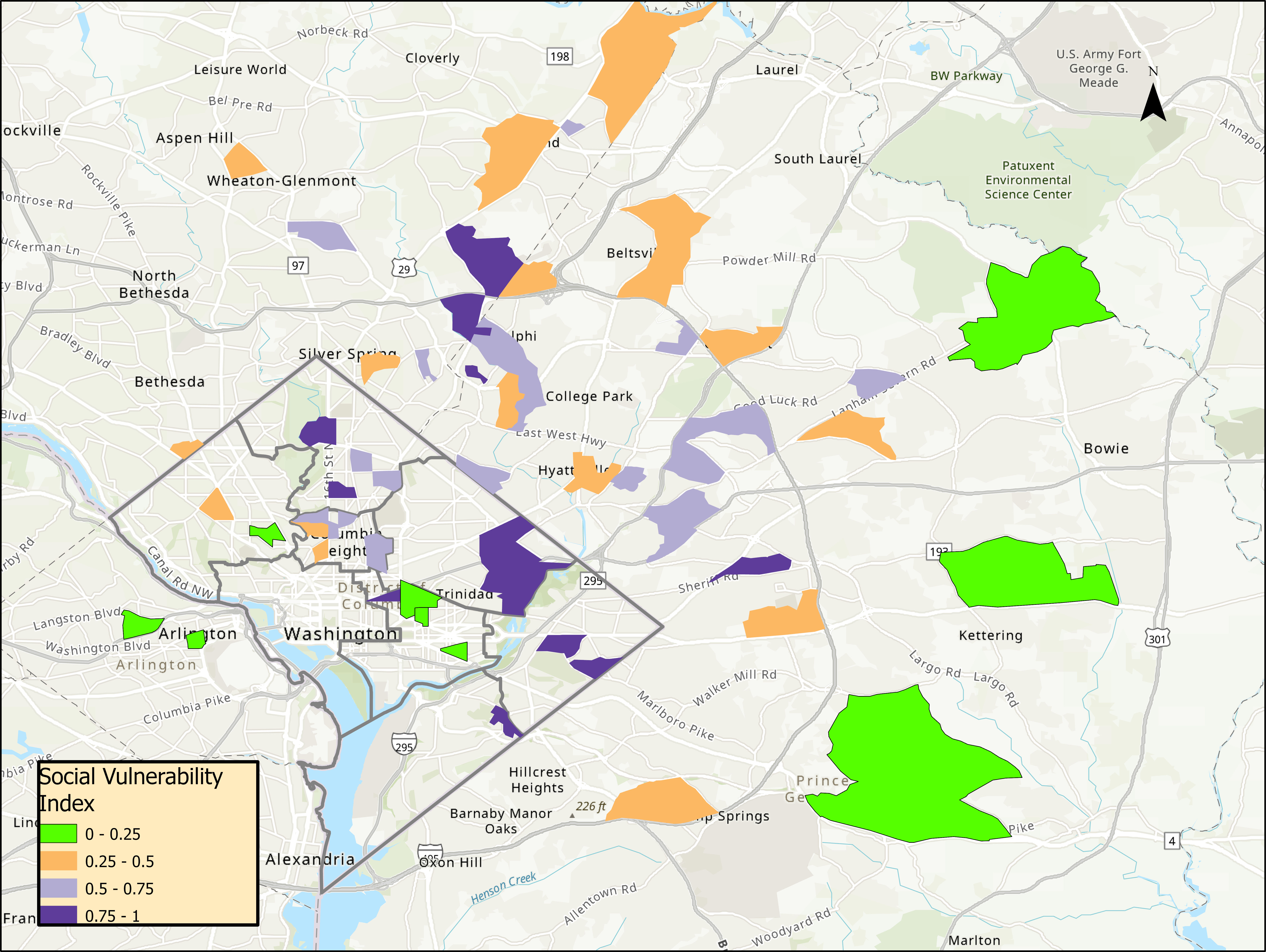
Results: We included 77 ESBL UTI cases and 233 controls. The geographic distribution of the ESBL UTI cases was identified in Figure 1. Significant hot spots for cases appeared in the northeast area (Figure 2). The association between SVI and ESBL UTI was not significant (Figure 3, OR 1.3, CI (0.4-4), p =0.7).
Conclusion(s): ESBL UTI has geographical significance in this preliminary study. ESBL UTI hot-spot distribution in the northeast area coincides with low-income neighborhoods where minority populations reside. No association was found between SVI and ESBL UTI. Further geographical analysis of risk factors will strengthen this case-control study.
.jpg)