Emergency Medicine: All Areas
Emergency Medicine 5 B
341 - Improving Emergency Preparedness in Pediatric Primary Care Offices: A Simulation-Based Multicenter Study
Publication Number: 341.209
- MY
Matthew Yuknis, MD, FAAP (he/him/his)
Assistant Professor of Clinical Pediatrics
Indiana University School of Medicine
Zionsville, Indiana, United States
Presenting Author(s)
Background:
Pediatric emergencies present to medical offices at variable frequencies, most often involving respiratory distress or seizures. Pediatric primary care offices are generally not well prepared to care for these situations, but improved preparedness scores have been linked to improved patient outcomes in other settings. In-situ simulation is a versatile tool for assessing clinical skills and latent safety threats in many settings.
Objective:
Using the existing American Academy of Pediatrics (AAP) policy statement on office emergency preparedness and in-situ simulation of common pediatric emergencies, the Improving Pediatric Acute Care Through Simulation (ImPACTS) group aimed to improve emergency preparedness in pediatric primary care offices.
Design/Methods:
This prospective, multi-center study assessed emergency preparedness and quality of care in pediatric primary care offices across academic medical centers (AMCs) throughout the United States. A collaborative hub/spoke framework was created between AMCs and offices with a central core supporting all hubs. During initial assessment, office preparedness was measured using a checklist derived from the existing AAP policy statement and quality of care during two simulations was measured via checklists developed by content experts in pediatric emergency and critical care medicine. Offices were provided a report of their performance and ImPACTS members worked with the office over 6-10 months to improve identified concerns. Offices were then re-assessed using the same checklists and scenarios. The program was piloted at 12 offices by 1 AMC prior to general enrollment.
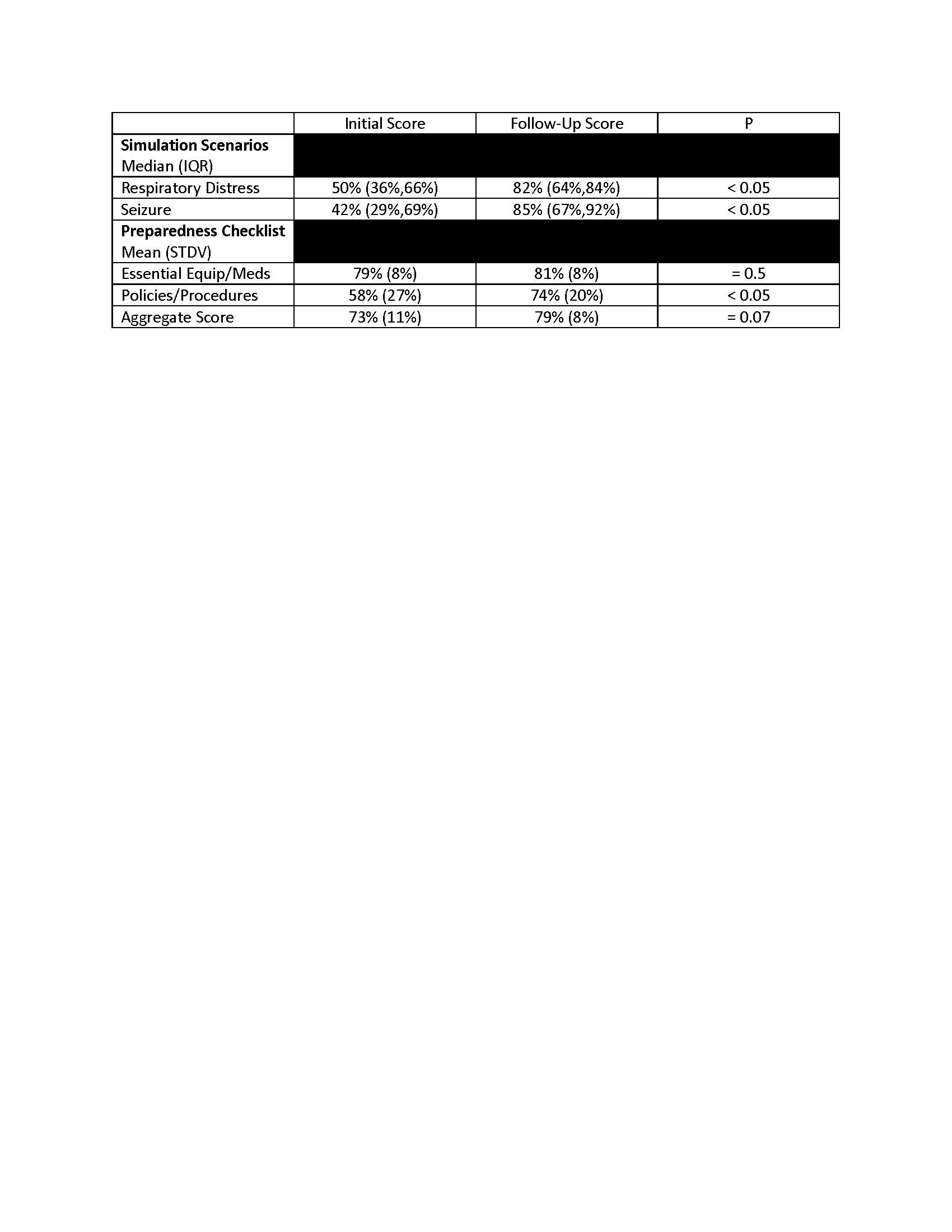
Results: Thirty-nine offices were recruited by 7 AMCs. Of these, 18 completed both preparedness surveys and 12 completed both simulations. Mean initial preparedness scores were 79% and 58% for essential equipment/medications and policies/procedures, with an aggregate score of 73%. Repeat scores were 81%, 74%, and 79%, respectively. Median initial simulation scores were 50% and 42% for the respiratory distress and seizure scenarios, with repeat scores of 82% and 85% respectively.
Conclusion(s):
The ImPACTs group formed successful collaboratives with multiple AMCs and primary care offices across the country. Improvement was noted in the policies/procedures portion of preparedness scores, as well as both simulation scores between first and second assessments. In the future, we plan to expand these efforts to more AMCs and office sites, including subspecialty offices and urgent visit centers. We also plan to use this data to revise existing policy regarding office emergency preparedness.