Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 4
428 - Association of pediatric CLABSI with race, ethnicity, and gender at a tertiary care hospital in the United States
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 428
Publication Number: 428.219
Publication Number: 428.219
Shreya Doshi, Children's National Health System, Washington DC, DC, United States; Deena Levey, Children's National Health System, Washington, DC, United States; Monica Monteon, Children's National Health System, Washington, DC, United States; Regan Trappler, Children's National, Washington, DC, United States; Michelle A. Liberty, Children's National Health System, Laurel, MD, United States; Annette Lee, Children's National Health System, Washington, DC, United States; Nada Harik, Children's National Health System, Washington, DC, United States; Xiaoyan Song, George Washington University School of Medicine and Health Sciences, Washington, DC, United States
Shreya Doshi, MBBS (she/her/hers)
Clinical fellow
Children's National Health System
Washington DC, District of Columbia, United States
Presenting Author(s)
Background: Modern healthcare in the United States (U.S.) continues to strive for equity in the process of delivering high quality and safe patient care for optimal patient outcomes. Central line-associated bloodstream infection (CLABSI) is widely accepted as a quality indicator and has been used to examine if equity is a factor causing healthcare-related disparities.
Objective: To evaluate the association of CLABSI with race and ethnicity over a 5-year period at a tertiary care pediatric hospital in the U.S.
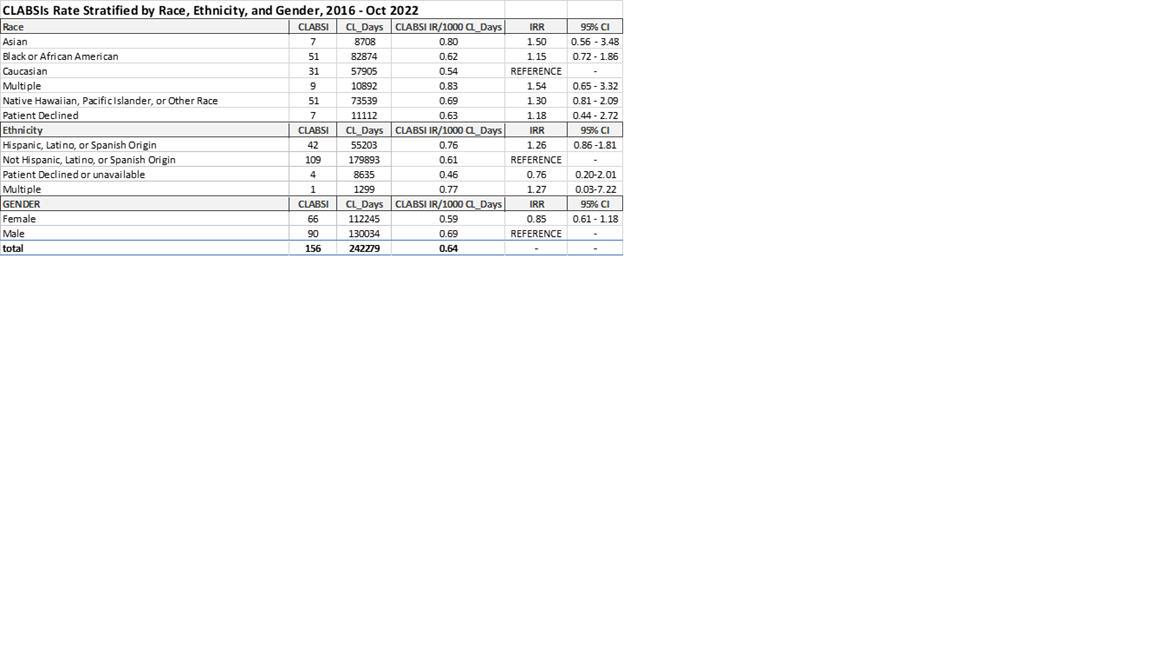
Design/Methods: This retrospective study was conducted from 1/1/2016 to 11/30/2022 at Children’s National Hospital in DC. The self-reported race and ethnicity were obtained from a database with data extracted from electronic medical record for administrative purpose. CLABSIs were identified by trained infection preventionists using the National Healthcare Safety Network definition. A CLABSI incidence rate (IR) was calculated as CLABSI per 1000 central line days (CL-D). CLABSI rates stratified by race, ethnicity, and gender were compared using Poisson regression analysis.
Results: The overall CLABSI IR was 0.64 per 1000 CL-D with 156 CLABSI events identified 242279 CL-D. Patients with self-reported multiple race or ethnicity had the highest CL-D, but the difference was not statistically significant by comparing to the reference groups of Caucasian or Not Hispanic, Latino, or Spanish Origin, respectively. The CLABSI IR in female was comparable with male patients.
Conclusion(s): Contrary to previous studies (Willer,2022 and McGrath,2021), we found no statistically significant association between CLASBSI and race, ethnicity, and gender. This may reflect on the practices at the hospital such as standardized central line care, safety culture, and DEI initiatives. This could also be a reflection of the demographics of the city where the hospital is located.