Medical Education: Simulation & Technology
Medical Education 6: Simulation & Technology 1
540 - Using a pediatric agitation pathway in simulation scenarios as a teaching module for providers in the pediatric emergency department
Publication Number: 540.228

Neehar Kundurti, MD (he/him/his)
Pediatric Emergency Medicine Fellow
University of New Mexico School of Medicine
Albuquerque, New Mexico, United States
Presenting Author(s)
Background:
Agitation is a leading cause of visits to the pediatric emergency department (PED). Until recently, there has been little guidance on management of acutely agitated pediatric patients in the PED, and no teaching modules exist to guide providers in clinical care.
Objective: This study aimed to develop and test a teaching module using two clinical simulations and a pediatric agitation pathway. We hypothesized that the module would improve provider knowledge and comfort in managing patients with acute agitation in the PED.
Design/Methods:
A pediatric agitation pathway was developed by a multidisciplinary team using consensus guidelines. The teaching module included two simulation case scenarios and the pediatric agitation pathway. Participants were emergency medicine residents, physician assistant residents and pediatric emergency medicine fellows.
Participants first completed a pre-intervention knowledge test and comfort survey. They were then introduced to the pediatric agitation pathway. Subsequently, they participated in two clinical case simulations and a debriefing session, followed by a post-intervention knowledge test and comfort survey. Power calculations indicated that with our expected sample size of 16 we would achieve a two-tailed power of 95% to detect a 1.0 standard deviation difference in pre/post-scores. Paired Wilcoxon signed-rank tests were used with an alpha threshold of 0.05.
Results:
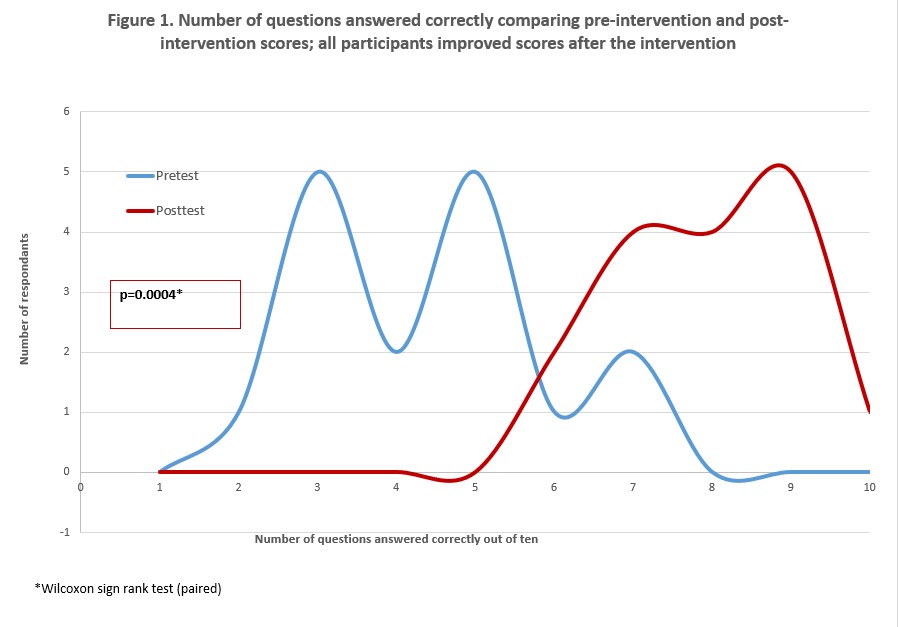
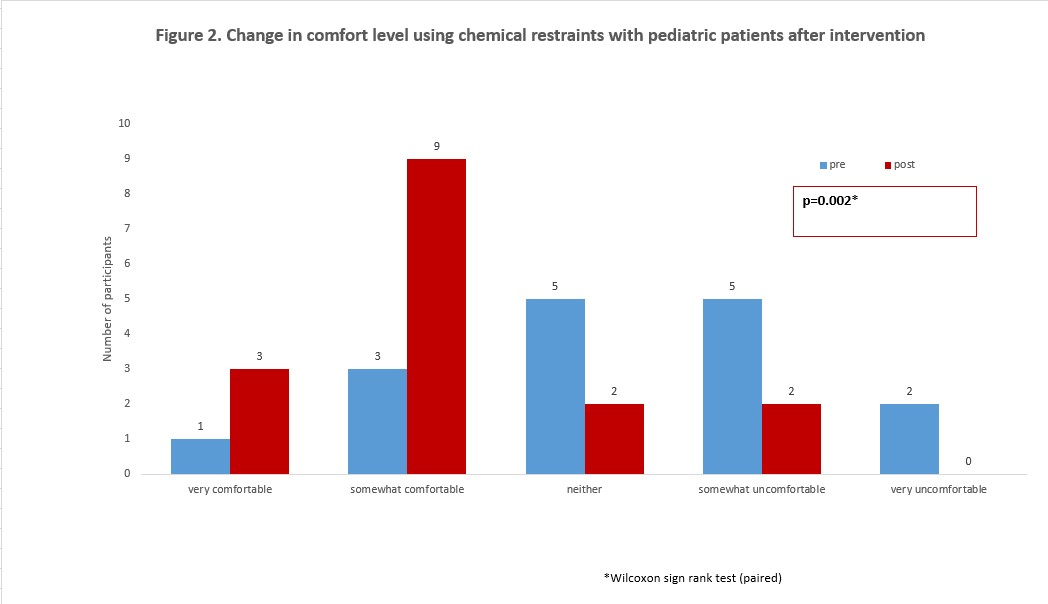
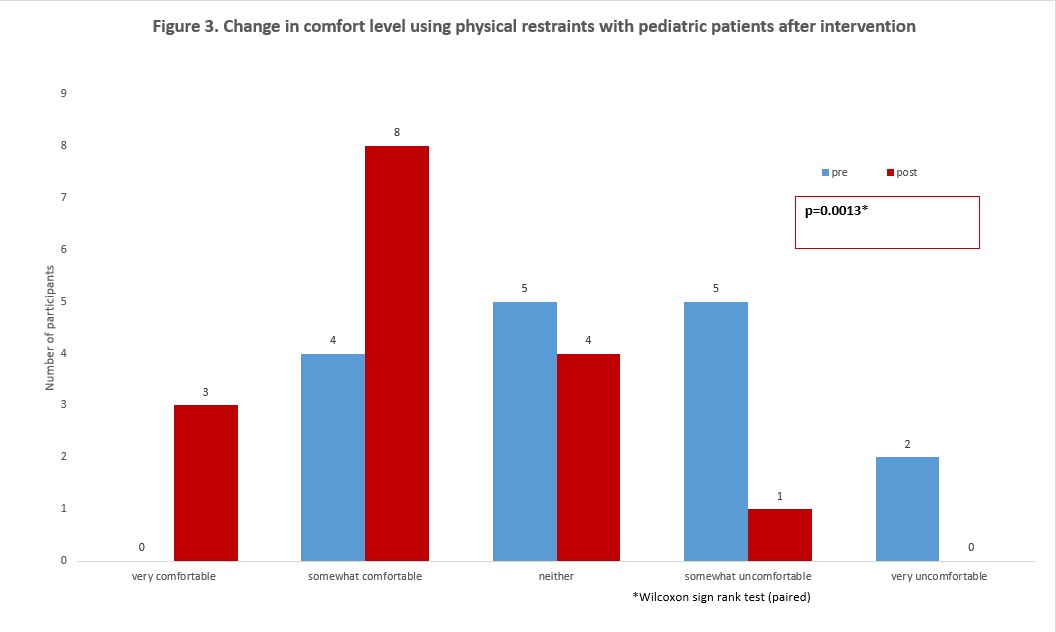
Sixteen participants completed the training. Overall knowledge improved after training (Figure 1; p=0.0004), as did comfort with use of chemical (Figure 2; p=0.002) and physical (Figure 3; p=0.013) restraints. The proportion of participants who answered correctly was higher for seven of the ten individual knowledge questions after the intervention. The number of questions answered correctly, or knowledge score, was 4.5 (inter-quartile range (IQR) 3, 5) pre-intervention and 8.0 (IQR 7, 9) post-intervention. The median knowledge score change was +4 out of 10 points (range +2, +5) (p=0.0004). All participants (100%) felt that the pediatric agitation pathway and teaching module would change their approach to using chemical restraints and would improve management of acute agitation in the PED.
Conclusion(s):
This teaching module, including a newly developed pediatric agitation pathway, was effective in improving overall knowledge and comfort associated with pediatric physical and chemical restraint use. The tool developed for this study fills a well-known need for provider training in how to manage agitation in the PED.