Emergency Medicine: All Areas
Emergency Medicine 5 B
337 - Clinical Practice Guideline Development, Implementation, and Assessment of Adherence in U.S. Pediatric Emergency Departments: A Cross-sectional Study
Publication Number: 337.209

Chidiebere V. Ugwu, MD (he/him/his)
Pediatric Emergency Medicine Fellow
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
Background:
Over the last decade, there has been an expansion of clinical practice guidelines (CPGs) to standardize and improve the care of children seen in pediatric emergency departments (PEDs). Appraisal of Guidelines for Research and Evaluation II (AGREE II) is a widely used tool to assess the quality and reporting of CPGs. However, adherence to AGREE II recommendations in CPGs developed in PEDs is unclear.
Objective:
To describe the process of CPG development, implementation, and assessment of adherence in PEDs in the United States.
Design/Methods:
In Oct-Nov 2022, we conducted a cross-sectional survey of CPGs developed in PEDs with fellowship programs. The survey was based on 12 questions used to assess the quality of CPG development in AGREE II. Employing a previously used threshold (Liu Y, et al. 2021), an AGREE II score ≥9 was classified as a high-quality CPG development process. Participant demographics, CPG implementation strategies, barriers, and methods of assessing adherence were collected via online survey using REDCap. Univariate analysis was used to assess associations.
Results:
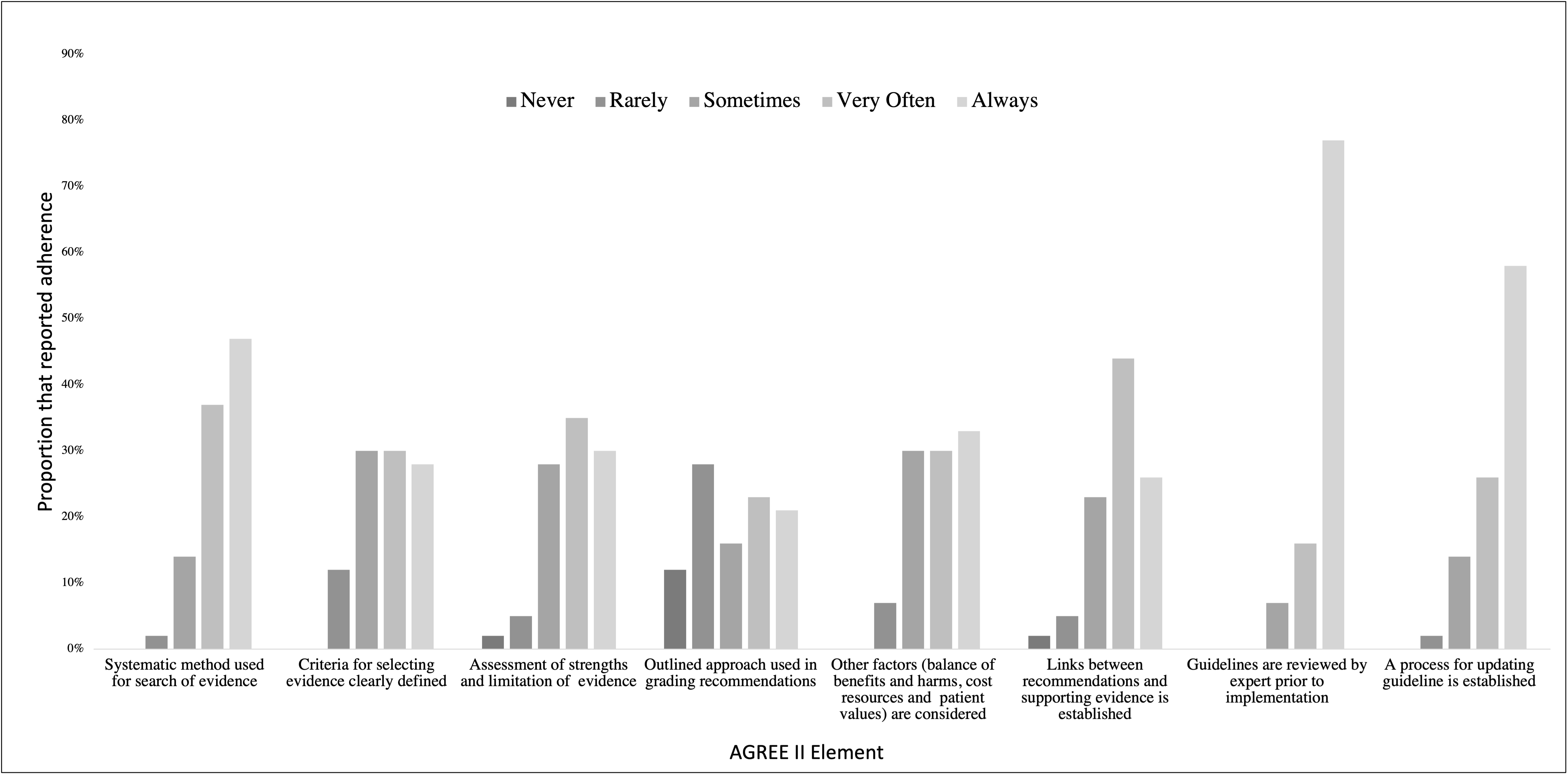
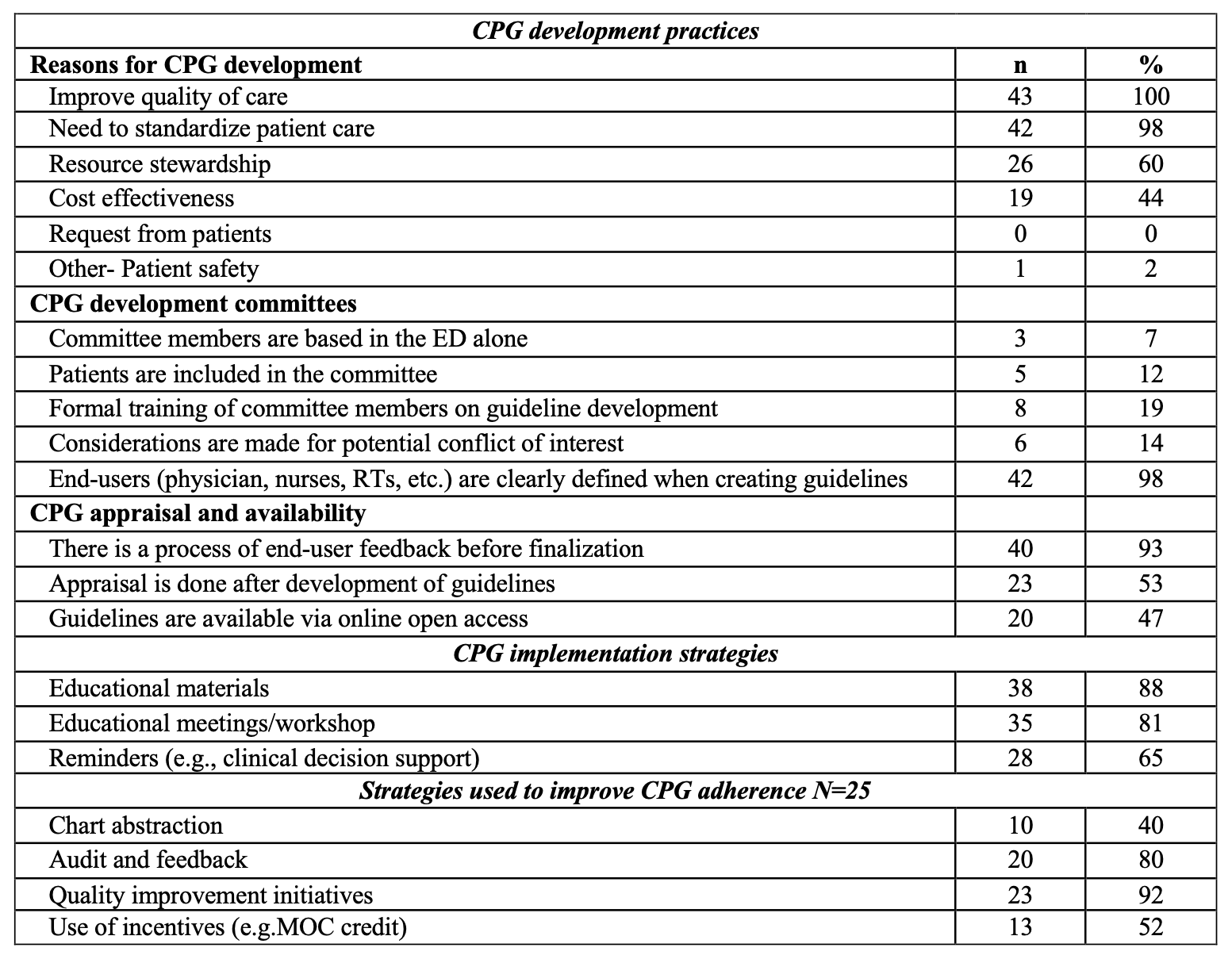
Respondents from 44/84 (52%) qualifying PEDs completed the survey. Most respondents (n=29, 66%) were from free-standing children’s hospitals and level 1 pediatric trauma centers (n=35, 79%). 43 (97%) PEDs in 28 states reported developing their own PED CPGs. The “need to improve quality of care” and “standardization of care” were the most common reasons for developing CPGs (Table). Only 19% reported receiving formal training on CPG development;12% reported including patients in CPG committees, and potential conflict of interest was infrequently considered (14%). Fewer than half (n=21, 49%) of PEDs had a high-quality CPG development process, often due to infrequent use of “an outlined approach for grading recommendations” (Figure). There was no association between the quality of CPG development process and ED volumes (P=0.42). Educational materials were reported as the most used strategy for CPG implementation while reminders (e.g. clinical decision support) were perceived to be most effective when used. Quality improvement initiatives, audits/feedback, and use of incentives (e.g. MOC credit) were commonly used to promote CPG adherence.
Conclusion(s):
Although a vast majority of surveyed PEDs develop their own CPGs, fewer than half reported developing CPGs through a high-quality process. Including patients on CPG committees, training on CPG development process, and a more rigorous approach towards grading evidence may promote higher quality CPGs and further improve clinical care for ill and injured children.