Mental Health
Mental Health 2
402 - Wrong Care in the Wrong Place: Pediatric Emergency Department Stakeholders’ Perspectives on the Behavioral and Mental Health Crisis in Connecticut
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 402
Publication Number: 402.231
Publication Number: 402.231
Michael P.. Goldman, Yale School of Medicine, New Haven, CT, United States; Noelle Frye, Yale New Haven Health System, New Haven, CT, United States; Mariann Kelley, Connecticut Children's Medical Center, West Hartford, CT, United States; Magna Dias, Yale School of Medicine, Orange, CT, United States; Kirsten Bechtel, Yale School of Medicine, New Haven, CT, United States; Megan L. petrucelli, Yale-New Haven Children's Hospital, Cromwell, CT, United States; Nanfi N. Lubogo, PATH CT, Cromwell, CT, United States; Marni McNiff, PATH CT, Brookfield, CT, United States; Mark Cicero, Yale School of Medicine, New Haven, CT, United States; Marc Auerbach, Yale University - Pediatrics And Emergency Medicine, New Haven, CT, United States; Steven C.. Rogers, Connecticut Children's, Hartford, CT, United States
- MG
Michael P. Goldman, MD (he/him/his)
Associate Professor of Pediatrics and Emergency Medicine
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Similar to other regions in the United States, Connecticut does not have a well-organized and easily accessible system to provide care to children with mental and/or behavioral health (MBH) problems. The COVID-19 pandemic exposed a failing system for children and families resulting in even more MBH crisis evaluations occurring in pediatric emergency departments (PEDs). These evaluations are time-intensive and most often result in discharge back into the community. Additionally they create bottlenecking and overcrowding, impacting the care of all PED patients, staff and general PED functionality.
Objective: To gain a deeper understanding of PED stakeholders’ perceptions of which MBH patients could safely receive care in non-emergent community settings. Additionally, we explored how the MBH crisis is impacting PED staff and PED function.
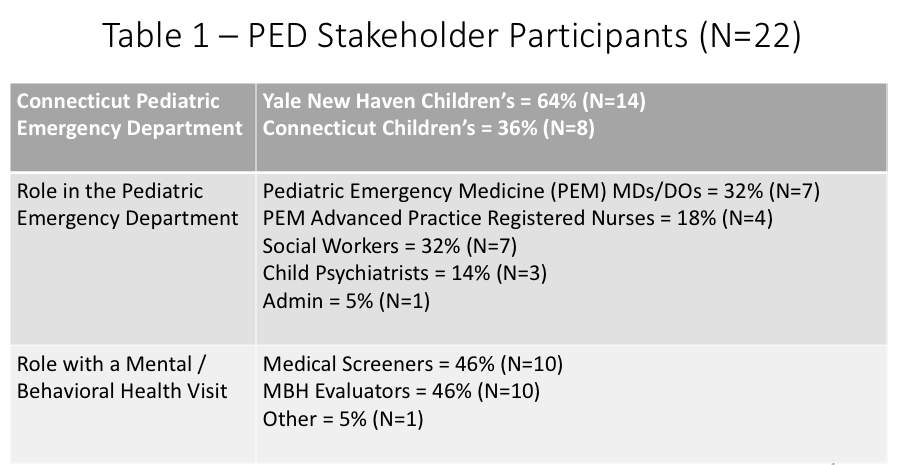
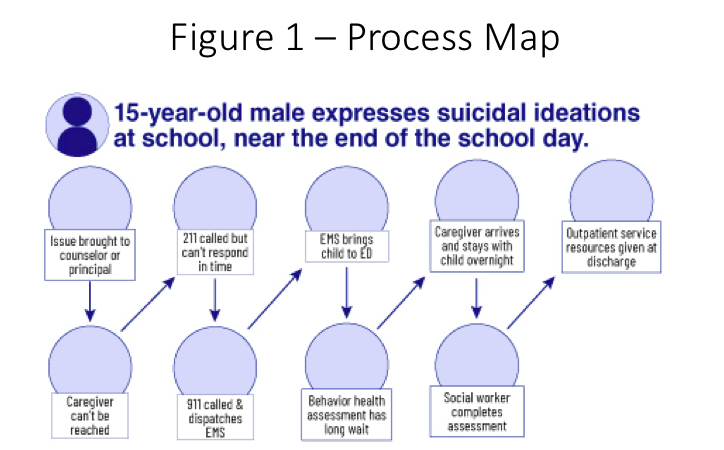
Design/Methods: We sought to interview key PED stakeholders regarding patients who are most frequently evaluated in the PED and subsequently discharged home. Targeted email recruitment for focus group participation was sent to the two PED MBH teams in our state. Groups were organized by MBH visit stakeholder role – medical screeners and MBH evaluators. Interviews were conducted, transcribed, independently coded and analyzed into themes through grounded theory’s constant comparative method. Findings were member checked. Process maps were generated.
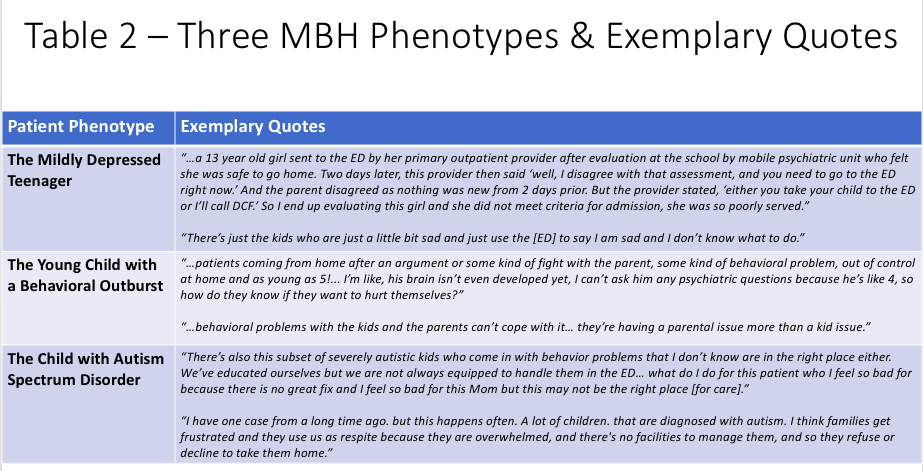
Results: Six focus groups included 22 participants (Table 1). In comparison to medical screeners, MBH evaluators were more accepting of the PED offering patients in crisis a brief respite from stressful stimuli, though all felt the PED was not a therapeutic environment. Consensus emerged for three phenotypes of patients that may be better served in the community -The mildly depressed teenager, the young child with a behavioral outburst and the child with autism (Table 2). Process maps outlined the steps these patients and families navigate, inclusive of their prolonged PED visit (Figure 1). Finally, all PED stakeholders reported moral injury, burnout and fear of missing both medical and MBH emergencies due to MBH crisis evaluation-induced PED overcrowding.
Conclusion(s): The MBH crisis exposed a dysfunctional “system of care” failing children, families and PEDs. These data offer focus to urgently needed interventions that may divert three common MBH patient populations away from PEDs. Critically important next steps include triangulation of our findings with the families of such MBH patients to ensure future interventions mutually benefit our patients and our PEDs.