Emergency Medicine: All Areas
Emergency Medicine 6
359 - Risk Factors Associated with Physical and Chemical Restraint Use in the Pediatric Emergency Department
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 359
Publication Number: 359.21
Publication Number: 359.21
Theresa T. Tran, University of Utah School of Medicine, Salt Lake City, UT, United States; Katharine Osborn, University of Utah School of Medicine, Salt Lake City, UT, United States; Taylor Blanding, University of Utah, Salt Lake City, UT, United States; Chong Zhang, University of Utah, MIDVALE, UT, United States; Roni D. Lane, University of Utah School of Medicine, Salt Lake City, UT, United States; David Chaulk, Primary Children's Hospital, Salt Lake City, UT, United States; Allison Neeley, Primary Children's Hospital, Salt Lake City, UT, United States

Theresa T. Tran, MD (she/her/hers)
Pediatric Emergency Medicine Fellow Physician
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Restraint use in the pediatric emergency department (PED) is prevalent. Although adult-based studies identify racial and gender disparities among patients undergoing physical restraint for aggression in the ED, there is limited literature on the pediatric population. To our knowledge, no studies evaluate the risk factors for chemical and/or physical restraints in pediatric patients with behavioral health concerns.
Objective: To evaluate risk factors associated with the use of physical and/or chemical restraints among patients who present with behavioral health concerns to the PED.
Design/Methods: Retrospective cross-sectional study at a free-standing, urban, quaternary, children’s hospital. We included patients 5 to 18-year-old who were seen in the PED for a behavioral health concern from January 2018 to June 2021. The main outcome was restraint use, defined as, (1) chemical, a medication administered to calm the patient and/or limit movement and (2) physical, soft-tie restraints to limit movement. We used logistic regression to evaluate the odds of restraint after adjustment for potential confounders.
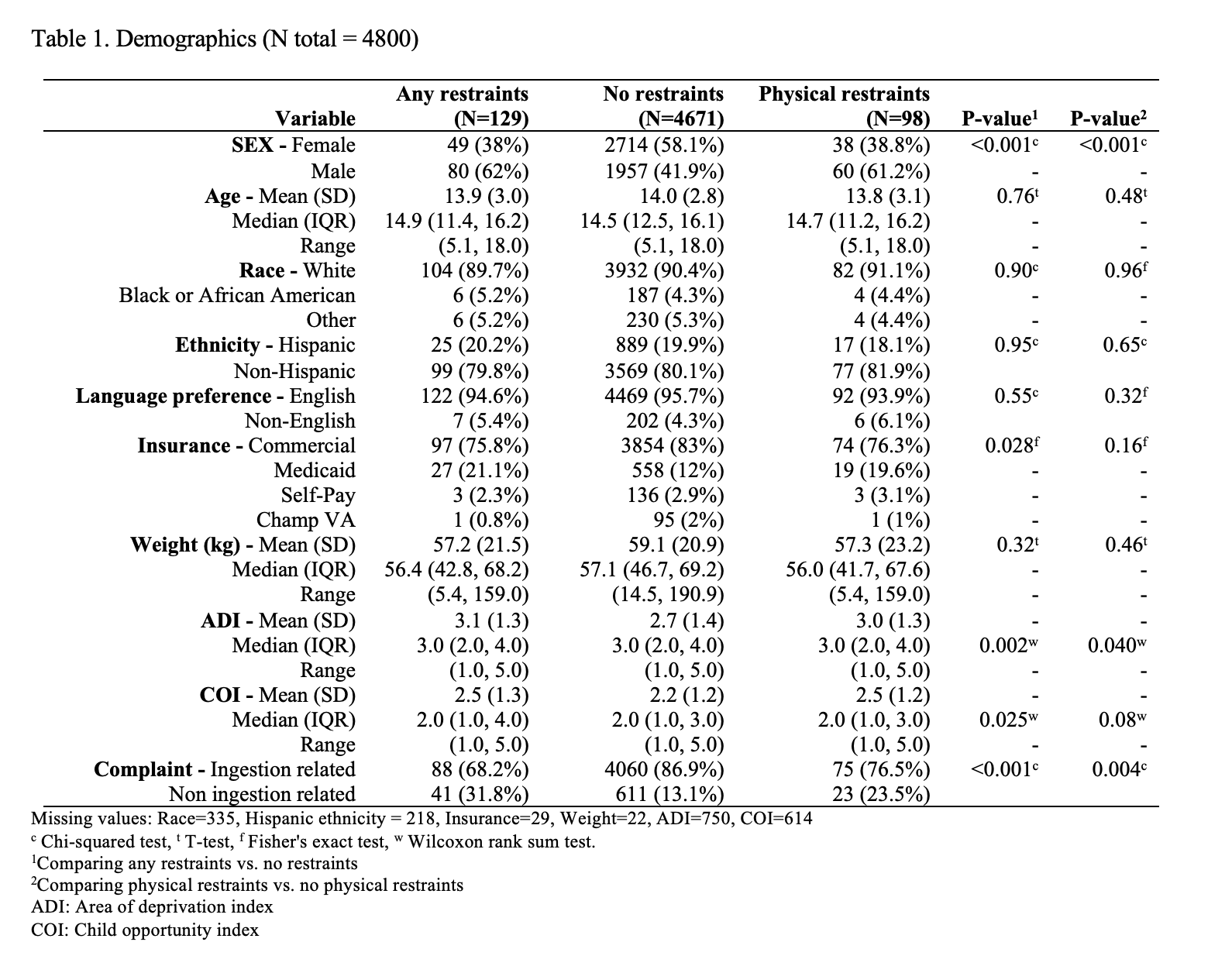
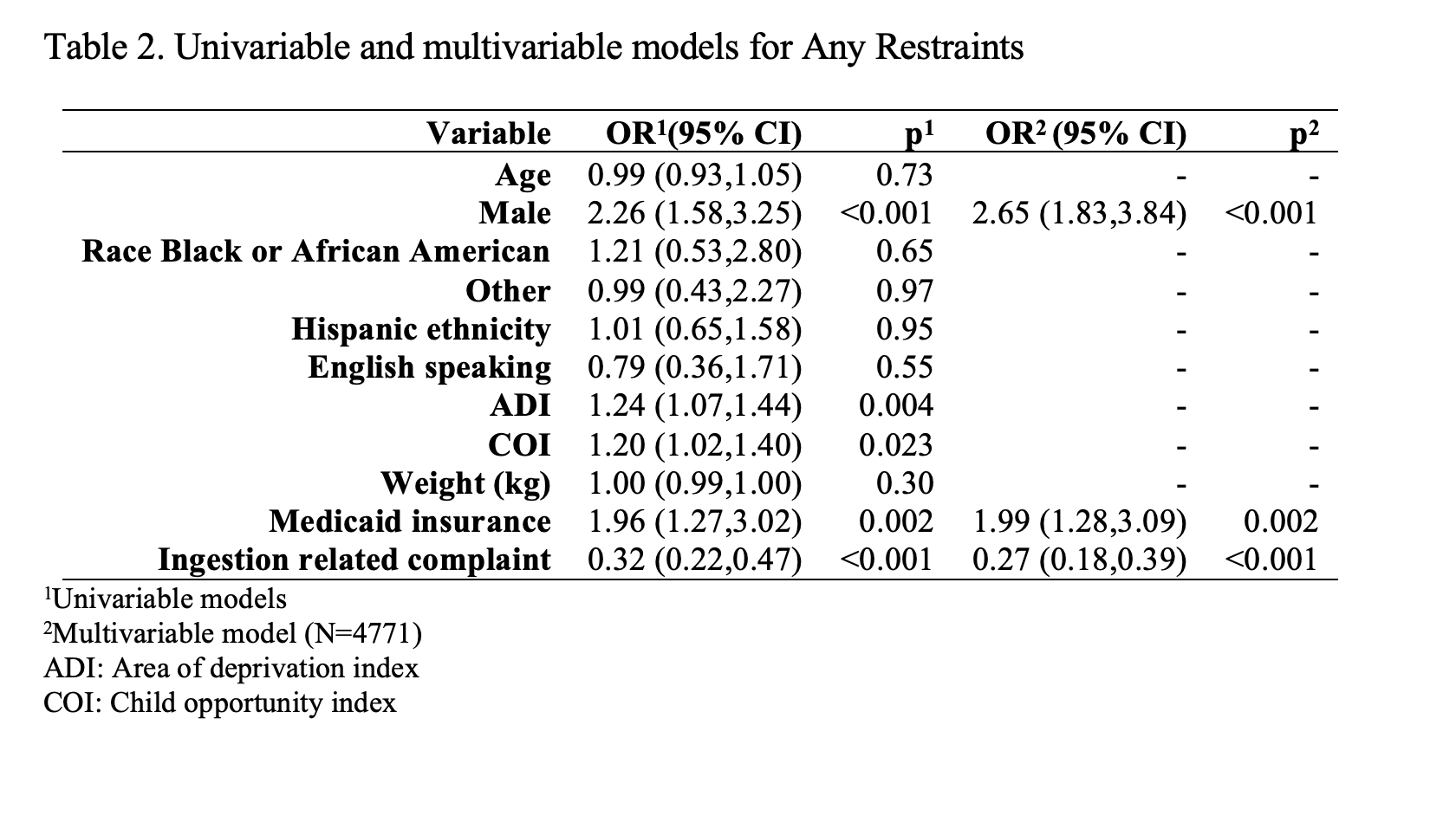
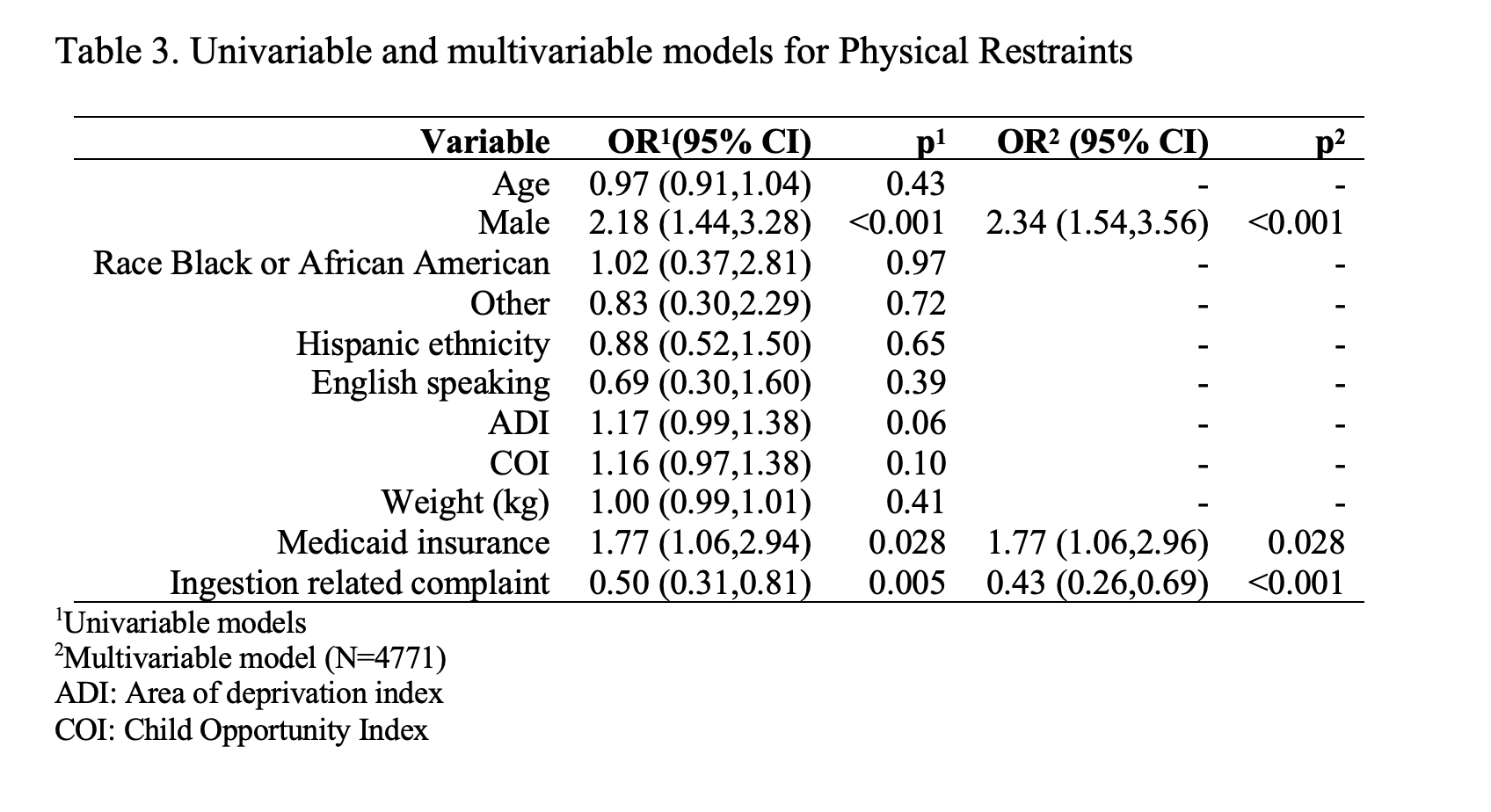
Results: During our study period, 4800 patients were seen for behavioral health concerns. Factors associated with increased restraint use were male sex and public insurance, odds ratio 2.65 (95% confidence interval [CI] 1.83, 3.84, p< 0.001) and odds ratio 1.99 (95% CI 1.28, 3.09, p< 0.002). Whereas, patients who presented with ingestion-related chief complaints were less likely to be restrained, odds ratio 0.27 (95% CI 0.18, 0.39, p< 0.001). These odds ratios are for any restraint, chemical and/or physical (see Table 2). The results for physical restraint, with and without chemical restraint, were similar (see Table 3). Descriptive data (Table 1) also showed an association of restraint with lower area of deprivation index (ADI) and child opportunity index (COI). There were no statistically significant differences for race, ethnicity, or language.
Conclusion(s): In this cohort of children presenting to the PED with a behavioral health concern, male sex and public health insurance were factors associated with restraint use. Providers generally do not know a patient’s insurance; therefore, the association may suggest an implicit bias towards other aspects of patients that are associated with insurance such as family income, socioeconomic status, or education level. This is supported by the lower values of ADI and COI also associated with restraints. Prospective studies may further elucidate specific factors of implicit bias and guide interventions to mitigate biases associated with restraint use in the PED.