Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 1
655 - NLRP3 Inflammasome-deficient Neonatal Mice Treated with Antibiotics may be Protected from Escherichia coli Sepsis-induced Acute Cerebral Inflammation
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 655
Publication Number: 655.24
Publication Number: 655.24
Esther M. Speer, Stony Brook Children's Hospital, Stony Brook, NY, United States; Amrendra Singh, Stony Brook Children's Hospital, Port Jefferson, NY, United States; Atilade Adedayo. Adedeji, Stony Brook University, Stony Brook, NY, United States

Esther M. Speer, MD
Associate Professor of Pediatrics
Stony Brook Children's Hospital
Stony Brook, New York, United States
Presenting Author(s)
Background: Neonatal sepsis triggers intense inflammatory responses involving inflammasome activation that contribute to mortality and brain injury, for which no effective therapy exists. The phosphodiesterase inhibitor pentoxifylline (PTX) is a candidate anti-inflammatory agent for newborn sepsis, however has limited inflammasome-suppressive properties. The effects of combined NLRP3 inflammasome suppression and PTX on cerebral inflammation in neonatal sepsis are unknown.
Objective: To determine the effects of NLRP3 inflammasome-deficiency (NLRP3-/-) on Escherichia coli-induced cerebral cytokine and chemokine concentrations in newborn mice in the presence or absence of gentamicin (GENT) or combined GENT and PTX (GENT+PTX).
Design/Methods: Newborn (< 24 hours (h) old) NLRP3-/- mice (B6.129S6-Nlrp3tm1Bhk/J; Jackson Laboratory, n=65) were injected intraperitoneally with live Escherichia coli K1 (105 colony forming units (CFU)/g weight) or an equal volume of saline for controls. After 1.5 hours (h), septic pups were randomly assigned to saline, GENT, or GENT+PTX, whereas controls received saline. Pups were euthanized after an additional 4 h, and CFUs, cytokines and chemokines were measured in homogenized brain tissue with multiplex immunoassays, and compared with 1-way ANOVA and Kruskal-Wallis tests.
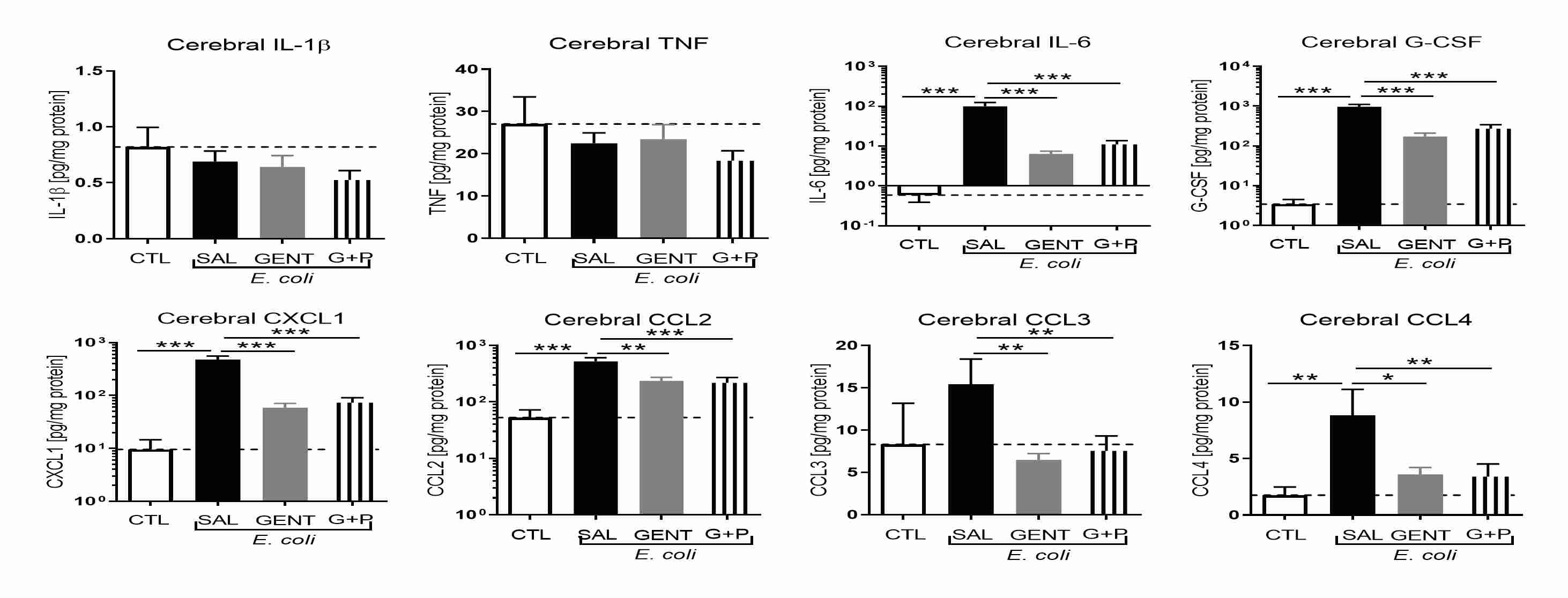
Results: Cerebral IL-1ß, TNF and IL-10 but not IL-6 were significantly lower in untreated E. coli-septic neonatal NLRP3-/- mice compared to our previous findings in wild-type C57BL/6J mice (Speer et al., Front Immunol 2020). Compared to controls, E. coli-septic untreated NLRP3-/- mice showed significantly higher cerebral IL-6, G-CSF, keratinocyte-derived chemokine (CXCL1), chemokine ligand 2 (CCL2), and CCL4 (p< 0.01), whereas TNF, IL-1ß, IL-12, and IL-10 did not increase. Addition of GENT and GENT+PTX suppressed E. coli-induced cerebral expression of IL-6, G-CSF, CXCL1, CCL2, CCL3, and CCL4 (p< 0.01) (Fig. 1). GENT+PTX diminished IL-17 compared to GENT alone (p< 0.05), however did not further decrease any other cytokines and chemokines. Cerebral tissue CFUs remained low in untreated and antibiotic-treated septic mice, and addition of PTX did not augment bacterial growth.
Conclusion(s): NLRP3-/- reduces sepsis-induced acute cerebral cytokines, which can be further diminished with antibiotic therapy, whereas addition of PTX provides only limited anti-inflammation. The NLRP3 inflammasome may be a promising future target to protect the neonatal brain from sepsis-induced inflammatory injury.