Medical Education: Resident
Medical Education 7: Resident 2
546 - Evaluating a Longitudinal Clinical Reasoning Curriculum for Pediatric Residents
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 546
Publication Number: 546.229
Publication Number: 546.229
James P. Bowen, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Molly C. Mack, UPMC Children's Hospital of Pittsburgh, Pittsburgh, PA, United States; Molly K. Marshall, The Mount Sinai Kravis Children's Hospital, New York, NY, United States; Jacob R. White, UPMC Children's Community Pediatrics, Pittsburgh, PA, United States; Catherine Polak, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Joanna Thomson, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States

Jimmy P. Bowen, MD (he/him/his)
Pediatric Hospital Medicine Fellow
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Clinical Reasoning (CR) skills are expected competencies assessed by the Accreditation Council for Graduate Medical Education (ACGME) Pediatric Milestones. Pediatric residents most often gain CR skills through informal experiential learning, with formal targeted education remaining inconsistent between clinical environments and residency programs.
Objective: To evaluate the impact of a CR curriculum on trainee comfort with CR skills and self-identified CR milestone level.
Design/Methods: We used Kern’s Six Steps for Curriculum Development to develop a CR curriculum for Pediatric residents at a children’s hospital. A needs assessment informed curriculum objectives: educate residents on common CR concepts and skills, allow practice of CR skills in case-based activities, and identify opportunities to apply CR skills clinically. The curriculum consisted of five morning report sessions led by Chief Residents. Pre- and post-implementation surveys assessed resident comfort with CR skills and their self-identified level on ACGME milestones related to CR skills. The post-survey also included questions assessing resident attitudes toward the sessions. Paired pre- and post-samples for comfort-based and milestone questions were analyzed using Wilcoxon Signed-Rank Tests. Questions regarding attitude towards sessions were dichotomized: strongly agree and agree vs. neither agree/disagree, disagree, and strongly disagree.
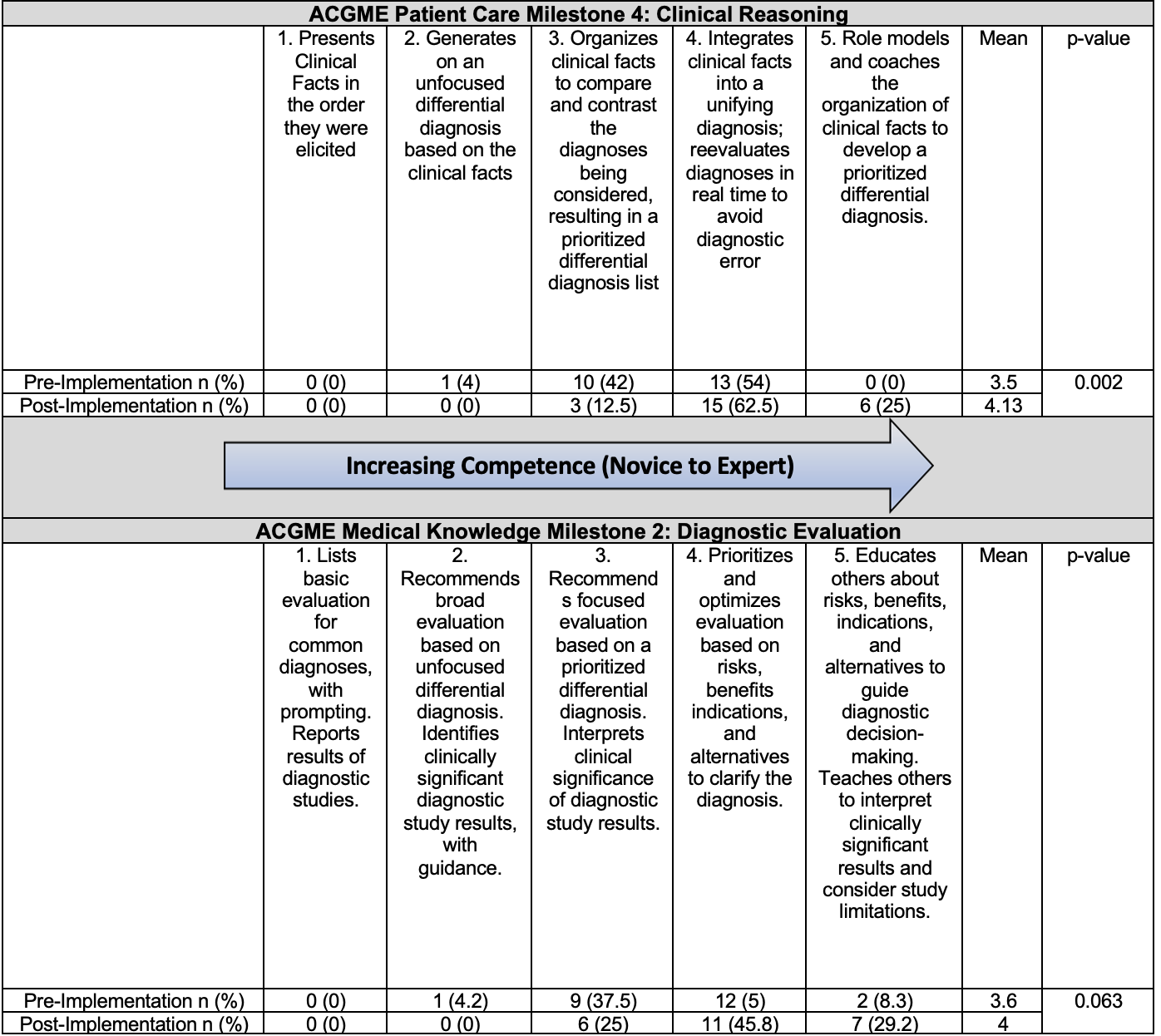
Results: Seventy-one trainees (24 PGY1 [59%], 27 PGY2 [66%], 20 PGY3 [56%]; 58% of total residency) completed the pre-survey. Fifty-one (18 PGY1 [44%], 16 PGY2 [39%], 17 PGY3 [47%]; 42% of total residency) completed the post-survey. Twenty-four (20% of total residency) paired samples were evaluated. Comfort in using CR skills increased (Table 1), including defining and using illness scripts, anticipating abnormal results, employing pathophysiology, and modifying differential diagnoses based on historical, physical exam, and laboratory findings. Self-assessment of ACGME milestones increased (Table 2). Most trainees who attended at least one session (n=44) reported finding the sessions helpful (n=43, 97%), relevant to their clinical work (n=43, 97%), and impactful to their clinical practice (n=32, 73%).
Conclusion(s): Following exposure to this pilot CR curriculum, pediatric residents reported increased comfort with all CR skills and self-identified level on the Milestone related to CR. The curriculum was well received. Dedicated CR education may advance understanding of and comfort using CR skills beyond what is gained with experiential learning alone.
.png)