Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 1
651 - Inflammatory and Endothelial Biomarkers in Early Onset Neonatal Sepsis
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 651
Publication Number: 651.24
Publication Number: 651.24
Jan Zivny, Charles University, 1st Medical Faculty, Prague, Praha 2, Hlavni mesto Praha, Czech Republic; Marek Mojzisek, University hospital in Motol, Prague 5, Hlavni mesto Praha, Czech Republic; Jan Janota, Charles Univerdity Prague, Praha 6, Hlavni mesto Praha, Czech Republic

Jan Zivny, MD, PhD
Associate professor
Charles University, 1st Medical Faculty, Prague
Praha 2, Hlavni mesto Praha, Czech Republic
Presenting Author(s)
Background: Mortality and morbidity of newborns can be improved by early targeted therapy. Search for innovative biomarkers that help the early diagnosis, assessment of severity and early treatment of perinatal complications including neonatal sepsis are priorities of current neonatology. Biomarkers of endothelial activation and injury represent a group of potential diagnostic markers of inflammatory diseases, such as early onset neonatal sepsis.
Objective: The aim of our study was to identify significant changes in potential inflammatory biomarkers in preterm newborns with early onset neonatal sepsis and systemic inflammatory response.
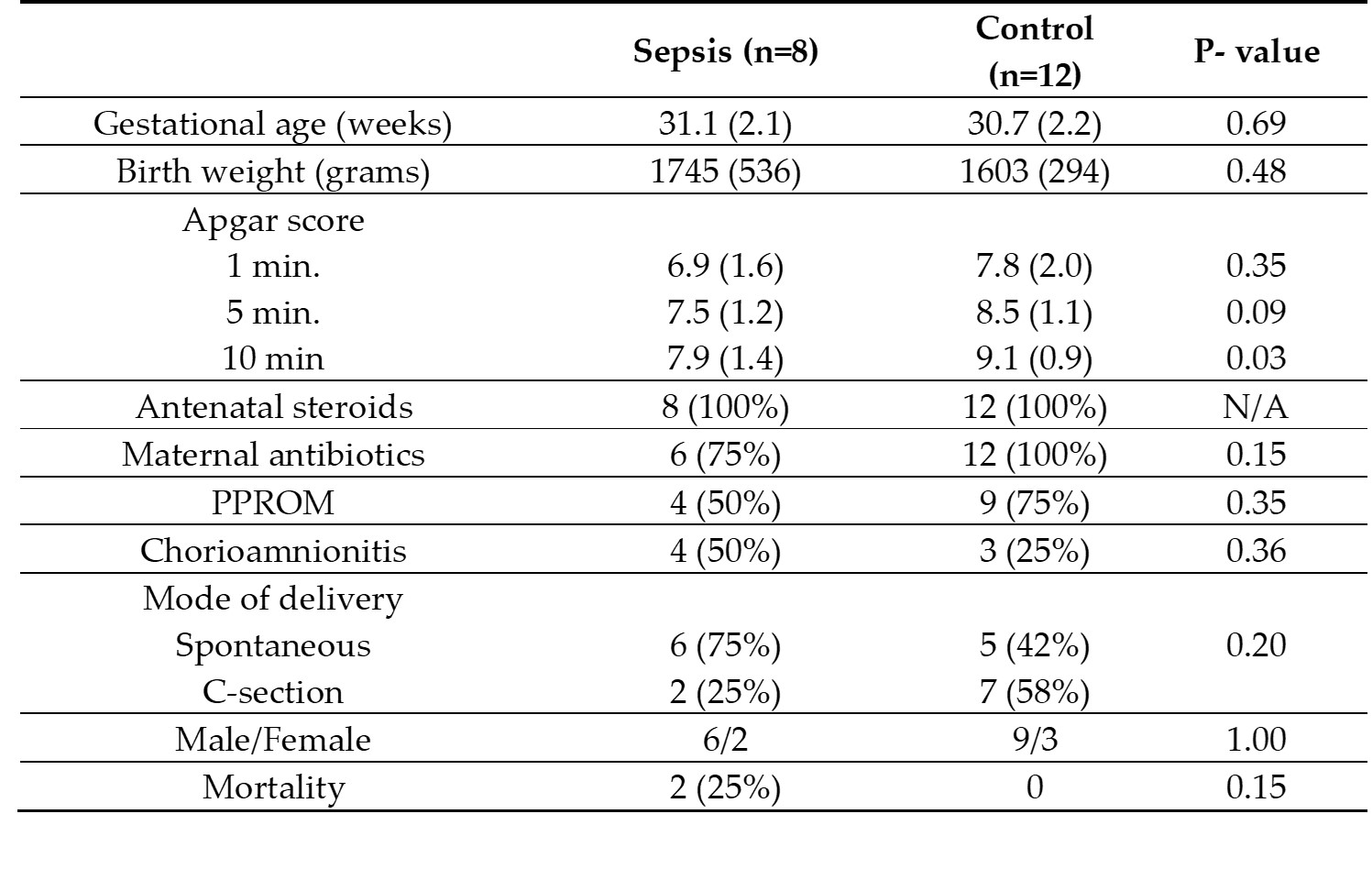
Design/Methods: The study group consisted of newborns with gestational age ≤ 32 weeks, with culture positive early onset neonatal sepsis (Sepsis group, n=8), and as a control group we enrolled newborns without sepsis (Control group, n=12). Soluble markers of inflammation (endocan, sICAM, sVCAM, sMadCAM, sVEGFR1, sVEGFR2, VEGF-A, angiopoietin 2, TNF, IL-1α, IL1β, IL-6, IL-18, endothelin 1) were measured using Luminex based multiplex assay. Cell membrane-derived large extracellular vesicles and endothelial cell-specific large extracellular vesicles were determined by flow cytometry.
Results: We found significant increase of interleukin 18 (IL-18) in cord blood of sepsis group (mean ± SEM; 104.7 ± 30.4 pg/mL vs. 52.7 ± 5.6 pg/mL; p = 0.02). In peripheral blood of sepsis group patients we found significant increase of VEGF-A compared to controls (196.0 ± 70.5 pg/mL vs. 59.6 ± 8.5 pg/mL, p = 0.02). In patient with early onset sepsis total large extracellular vesicle concentration was increased, while the endothelium specific vesicles were decreased compared to gestation age and weight matched healthy control.
Conclusion(s): In conclusion, we found that in early onset neonatal sepsis IL-18 and VEGF-A might be considered in diagnostic workup. Endothelial-specific large extracellular vesicles may not contribute to the increased concentration of large extracellular vesicles associated with early onset neonatal sepsis.
.jpg)
