Critical Care
Critical Care 2
315 - Risk Factors for Central Line-Associated Bloodstream Infection in the Pediatric ICU Despite Standard Prevention Measures
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 315
Publication Number: 315.205
Publication Number: 315.205
Kaitlyn Marks, Boston Children's Hospital, Jamacia Plain, MA, United States; Katherine Rosengard, Boston Children's Hospital, Boston, MA, United States; Jennifer D. Franks, Boston Children's Hospital, Southborough, MA, United States; Steven Staffa, Boston Children's Hospital, Boston, MA, United States; Jenny Chan Yuen, Boston Children's Hospital, Boston, MA, United States; Jeffrey P. Burns, Harvard Medical School, Boston, MA, United States; Gregory P. Priebe, Boston Children's Hospital, Boston, MA, United States; Thomas J. Sandora, Boston Children's Hospital, Boston, MA, United States

Kaitlyn Marks, MD (she/her/hers)
Clinical Fellow
Boston Children's Hospital
Jamacia Plain, Massachusetts, United States
Presenting Author(s)
Background: Central line-associated bloodstream infections (CLABSI) continue to be a leading cause of morbidity and mortality in pediatric intensive care unit (ICU) patients despite high compliance with recommended prevention bundles for line insertion and maintenance.
Objective: To identify risk factors for the development of CLABSI in the pediatric intensive care setting in an era with high adherence to standard prevention measures.
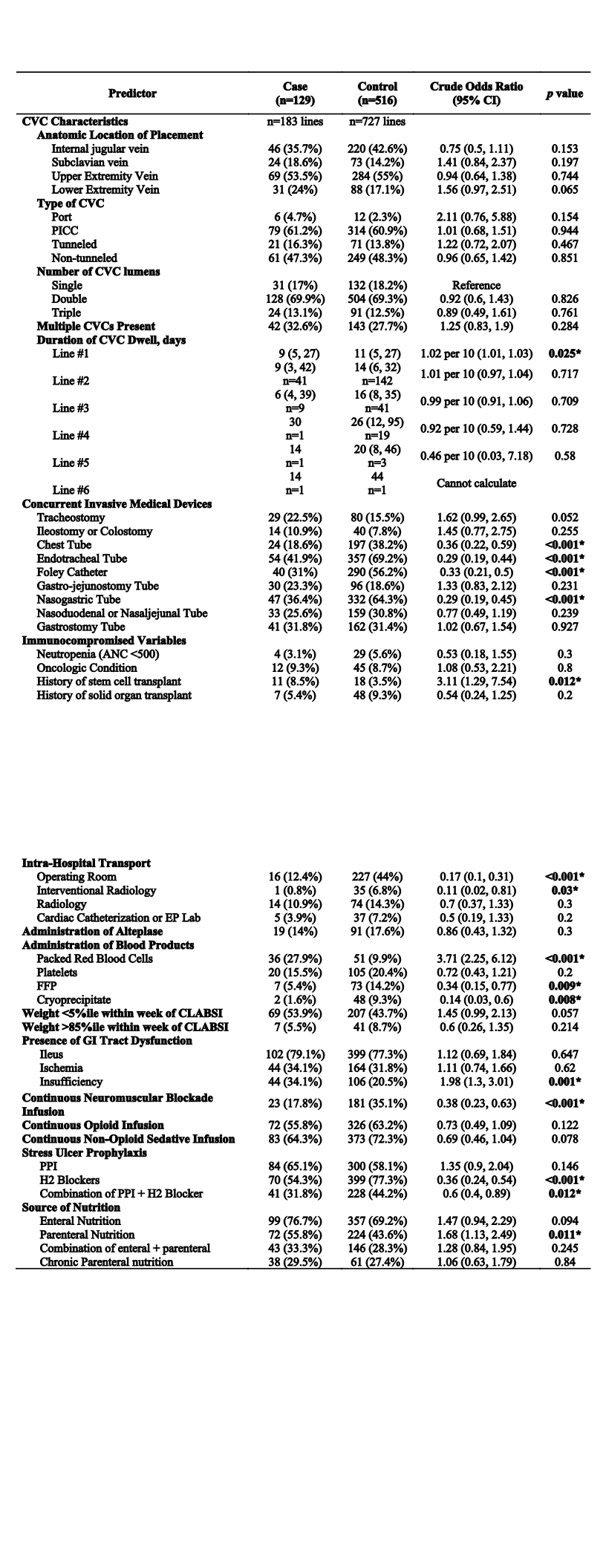
Design/Methods: Retrospective matched case-control study from January 1, 2015 through December 31, 2020. Cases had a CLABSI and were identified via an Infection Prevention database among inpatients in one of four ICUs at Boston Children’s Hospital. Controls were inpatients in one of the four ICUs for ≥ 2 days with a central venous catheter (CVC) in place for ≥ 2 days who did not develop a CLABSI. Controls were matched 1:4 on ICU of admission and admission date (± one calendar month). Multivariable conditional logistic regression was used to identify independent risk factors for CLABSI while accounting for clustering within matched sets.
Results: In total, 129 cases were matched to 516 controls. Case patients had a significantly longer duration of ICU stay (median 45.7 days vs. 8.8 days, P < 0.001) and higher mortality rate (20.9% vs. 8.7%, P < 0.001) compared with controls. Cases were admitted to the cardiac ICU (n=42, 32.6%), medical/surgical ICU (n=50, 38.8%), medical ICU (n=21, 16.3%), and neonatal ICU (n=16, 12.4%). CVC maintenance bundle compliance across all four ICUs during the study period was approximately 80%. Independent risk factors for CLABSI included administration of packed red blood cells (adjusted odds ratio (aOR) 6.05, 95%CI [2.97, 12.3], P < 0.001) and receiving parenteral nutrition (aOR 2.31, 95%CI [1.23, 4.33], P=0.009). Variables significantly associated with a lower odds of CLABSI in multivariable analysis included continuous neuromuscular blockade (aOR 0.32, P< 0.001), intrahospital transport to the operating room (aOR 0.17, P< 0.001) or to interventional radiology (aOR 0.06, P=0.027), administration of histamine H2-receptor-blocking medications (aOR 0.36, P=0.003), presence of a nasogastric tube (aOR 0.34, P< 0.001) and presence of an endotracheal tube (aOR 0.42, P=0.01).
Conclusion(s): Pediatric ICU patients receiving packed red blood cells and parenteral nutrition are at risk for CLABSI despite high but imperfect adherence to current prevention measures. Improving reliability around current prevention measures and developing novel strategies to further reduce CLABSI risk in the current era should be prioritized.
.jpg)
.jpg)
