Hematology/Oncology
Hematology/Oncology 2
158 - Pediatric oncology multidisciplinary provider perspectives on chemotherapy-induced nausea and vomiting (CINV) management and preferred improvement approaches
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 158
Publication Number: 158.22
Publication Number: 158.22
Hadley Bloomhardt, Boston Children's Hospital/Harvard Medical School, Boston, MA, United States; Melissa Rubin, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Yanling Xue, Columbia University, New York, NY, United States; Zhezhen Jin, Columbia University, New York, NY, United States; Laura Masino, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Nobuko Hijiya, Columbia University Vagelos College of Physicians and Surgeons, new york, NY, United States; Melissa P.. Beauchemin, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States

Melissa Rubin, MD (she/her/hers)
Resident
NewYork-Presbyterian Morgan Stanley Children's Hospital
New York, New York, United States
Presenting Author(s)
Background: Chemotherapy-induced nausea and vomiting (CINV) is common in children undergoing cancer treatment, and significantly impacts quality of life. Clinical practice guidelines (CPGs) have been developed to guide CINV management, though many patients do not receive guideline-concordant care. Few studies have examined provider perspectives on CINV management or preferred improvement approaches.
Objective: To characterize pediatric oncology (PO) multidisciplinary provider perception of CINV control in their patients and knowledge around CINV CPGs, and to assess interest in approaches to improve CINV management.
Design/Methods: We conducted a cross-sectional study of PO providers, including chemotherapy prescribers (attendings, fellows, nurse practitioners (NPs)), pediatric residents, and nurses (RNs), at a large freestanding children’s hospital. Providers completed an anonymous online survey about CINV control in patients admitted for scheduled chemotherapy during their most recent week on service, and their knowledge and utilization of CINV CPGs. Data was analyzed using Stata 14.2.
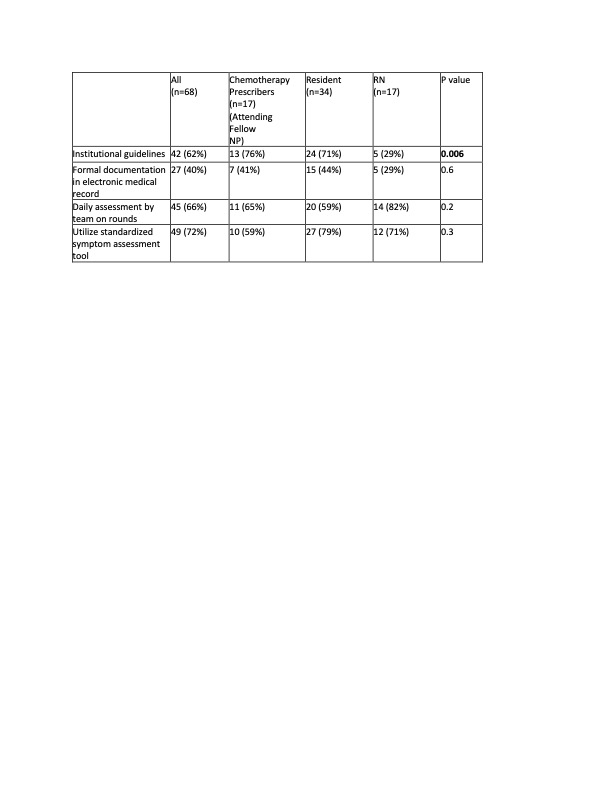
Results: The survey was distributed to 155 PO providers with a response rate of 44% (17 chemotherapy prescribers, 34 residents, 17 RNs). Overall, 75% of respondents felt CINV management could be moderately/extremely improved, significantly more so by non-RNs (82% chemotherapy prescribers, 82% residents, 53% RNs, p=0.02). Additionally, 35% of providers perceived CINV was not well/slightly well treated. Over half of respondents did not have awareness of CINV CPGs, particularly residents (88%, vs. chemotherapy prescribers 18% and RNs 59%, p< 0.001). Most residents felt not comfortable/somewhat comfortable ordering medications to prevent (79%) and treat (59%) CINV. Only 5% of residents reported utilizing CPGs to learn about CINV management; only 13% of chemotherapy prescribers used CPGs as a resource for ordering antiemetic regimens. Interest in methods to improve CINV management varied by provider type (Table 1), with greatest interest in a standardized CINV assessment tool (72%) and daily assessment on rounds (66%).
Conclusion(s): In this study, PO providers reported that CINV management can be improved. Many front-line providers did not feel comfortable managing CINV, and few providers used CPGs to determine treatment. Implementing education in this area may help to improve provider comfort and, ultimately, the patient experience. Providers were interested in several interventions to improve CINV management. Future studies will develop and evaluate CINV management interventions.