Emergency Medicine: Quality Improvement
Emergency Medicine 5 B
336 - Avoid the Radiation: Optimizing Utilization of Computed Tomography Imaging for Pediatric Appendicitis
Publication Number: 336.209

Jennifer Overfield, MD (she/her/hers)
Pediatric Resident
Monroe Carell Jr. Children's Hospital at Vanderbilt
Nashville, Tennessee, United States
Presenting Author(s)
Background:
Appendicitis is a common pediatric surgical emergency, and computed tomography (CT) is overused in diagnosing pediatric appendicitis. Our institutional rates of CT utilization for suspected appendicitis are higher than peer participants in the NSQIP-P Pediatric Surgery Quality Collaborative.
Objective: We aimed to reduce CT utilization in the diagnostic evaluation of pediatric appendicitis from 32% to the NSQIP-P benchmark of 15% by 6/2022.
Design/Methods:
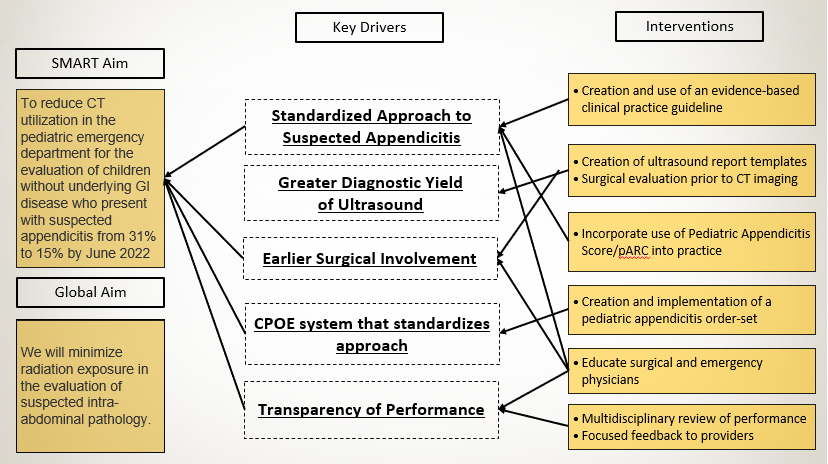
Retrospective chart review was done for baseline data from 1/2021- 8/2021 and followed prospectively. Patients in the pediatric emergency department (ED) were identified based on ICD-10 codes for abdominal pain and acute appendicitis. A multidisciplinary team formed in 6/2021 and developed a key driver diagram (Figure 1). A clinical practice guideline (CPG) utilizing the Pediatric Appendicitis Score was developed in 9/2021 and trialed in the clinical setting. The CPG was institutionally published in 12/2021 with accompanying education and a complaint-based order set embedded in the electronic medical record for clinical decision support. The primary outcome was percent of patients with CT scan. Timing of surgical consultation and radiology template use were process measures. Balancing measures were negative-pathology appendectomies (NPA) and ED return visits within 72 hours with subsequent appendicitis diagnosis. Data were analyzed using statistical process control charts and Nelson rules to detect special cause variation.
Results:
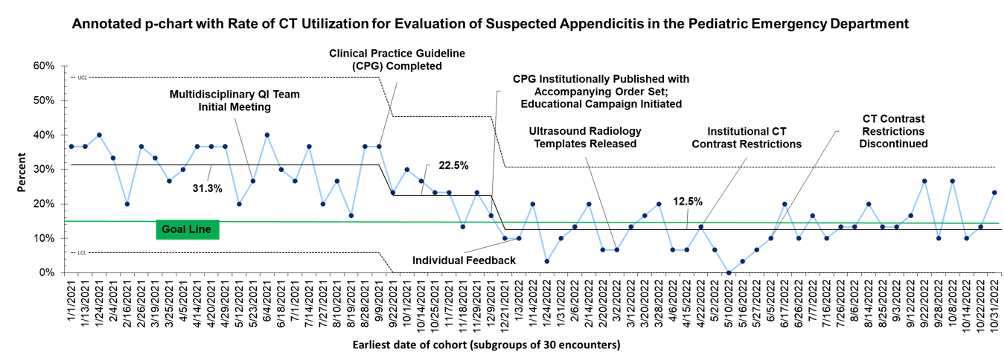
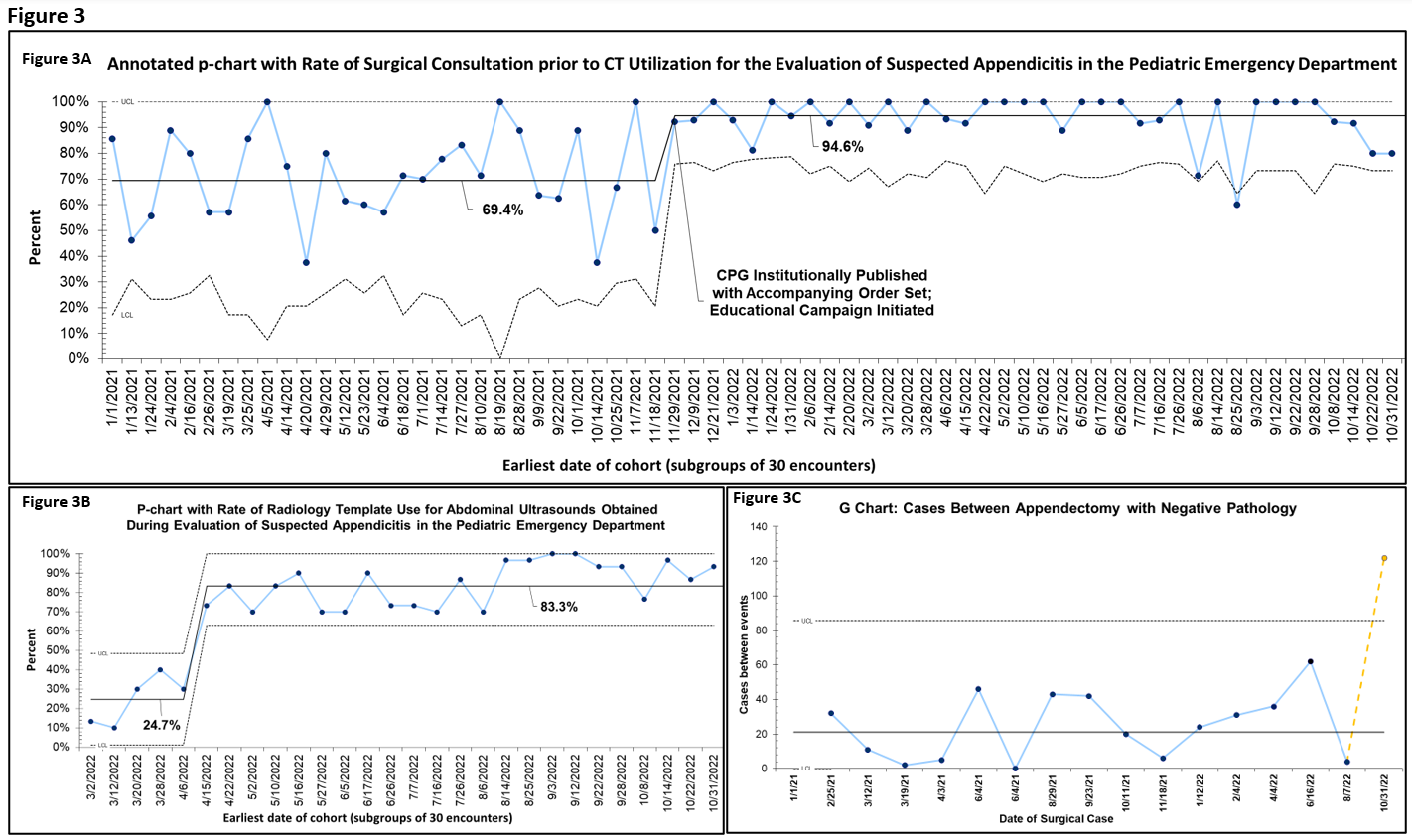
The cohort included 2010 total encounters, 624 of which represented the baseline with a CT rate of 31.3%. Following multiple PDSA cycles to develop and test the CPG, special cause variation was detected in CT use to 22.5%. Order set launch was also associated with special cause variation resulting in a centerline shift to 12.1% that has been sustained for 10 months (Figure 2). Rate of surgical consultation prior to CT imaging increased from 69.4% to 94.6% (Figure 3a) and radiology template use increased from 24.6% to 83.3% (3b). There was one ED return visit within 72 hours. Special cause variation in NPA was appreciated in 10/2022, with a decreasing frequency of NPA, indicating more cases between these rare events (3c).
Conclusion(s):
CT imaging was safely reduced in the workup of pediatric appendicitis. Workflow standardization with the use of a CPG and order set, along with earlier involvement of the surgical team, facilitated the reduction in CT utilization. Ongoing efforts include standardizing surgical serial exams and continuous performance review.