Medical Education: Resident
Medical Education 7: Resident 2
552 - Prioritizing Health Literacy Competencies for Pediatric Residents - A Modified Delphi Study
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 552
Publication Number: 552.229
Publication Number: 552.229
Nicole K. Meyers, New York Presbyterian Hospital - Columbia University Medical Center, New York, NY, United States; Mary Ann Abrams, The Ohio State University College of Medicine, Columbus, OH, United States; Suzanne Friedman, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Marguerite Costich, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Aditi Gupta, Baylor College of Medicine, Houston, TX, United States; Andrea K.. Morrison, Medical College of Wisconsin, Milwaukee, WI, United States; Margaret Wood, Baylor College of Medicine, Houston, TX, United States; Joy Solano, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States
Nicole K. Meyers, MD (she/her/hers)
Pediatric Chief Resident
New York Presbyterian Hospital - Columbia University Medical Center
New York, New York, United States
Presenting Author(s)
Background: Improving providers’ ability to use health literate communication is considered foundational in Healthy People 2030. This is imperative in pediatrics given that low health literacy is prevalent among parents and associated with poor health outcomes among their children. There is currently no consensus on a standardized health literacy curriculum for use in pediatric residency programs.
Objective: We sought to establish consensus on competencies needed to train pediatric residents in health literacy.
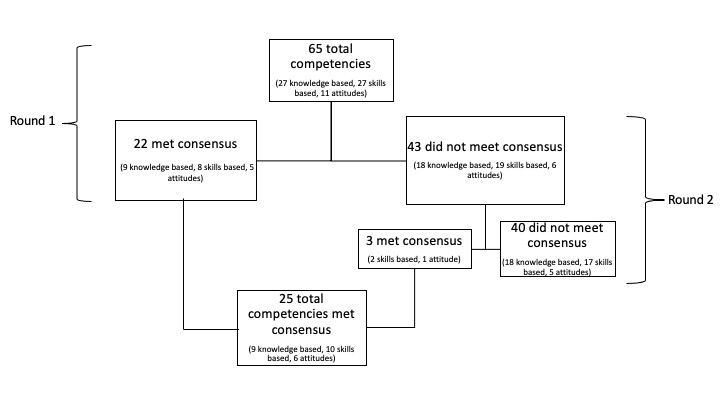
Design/Methods: We used modified Delphi methodology to establish consensus around a previously published set of health literacy competencies for family medicine residents. These competencies were reviewed at the outset by study group members to ensure they were comprehensive. Members of the Academic Pediatric Association (APA) Health Literacy Special Interest Group recommended experts based on their experience in pediatric health literacy research and/or education to serve as panelists. Panelists classified each competency as essential, recommended, neutral, or not recommended, and provided free-text comments that were integrated into final development of the competencies. Consensus was defined a priori as >70% of panelists identifying a competency as essential, or 100% of panelists agreeing that a competency was recommended or essential. Two survey rounds have been completed with sharing of anonymous first round responses during the second round (Figure 1).
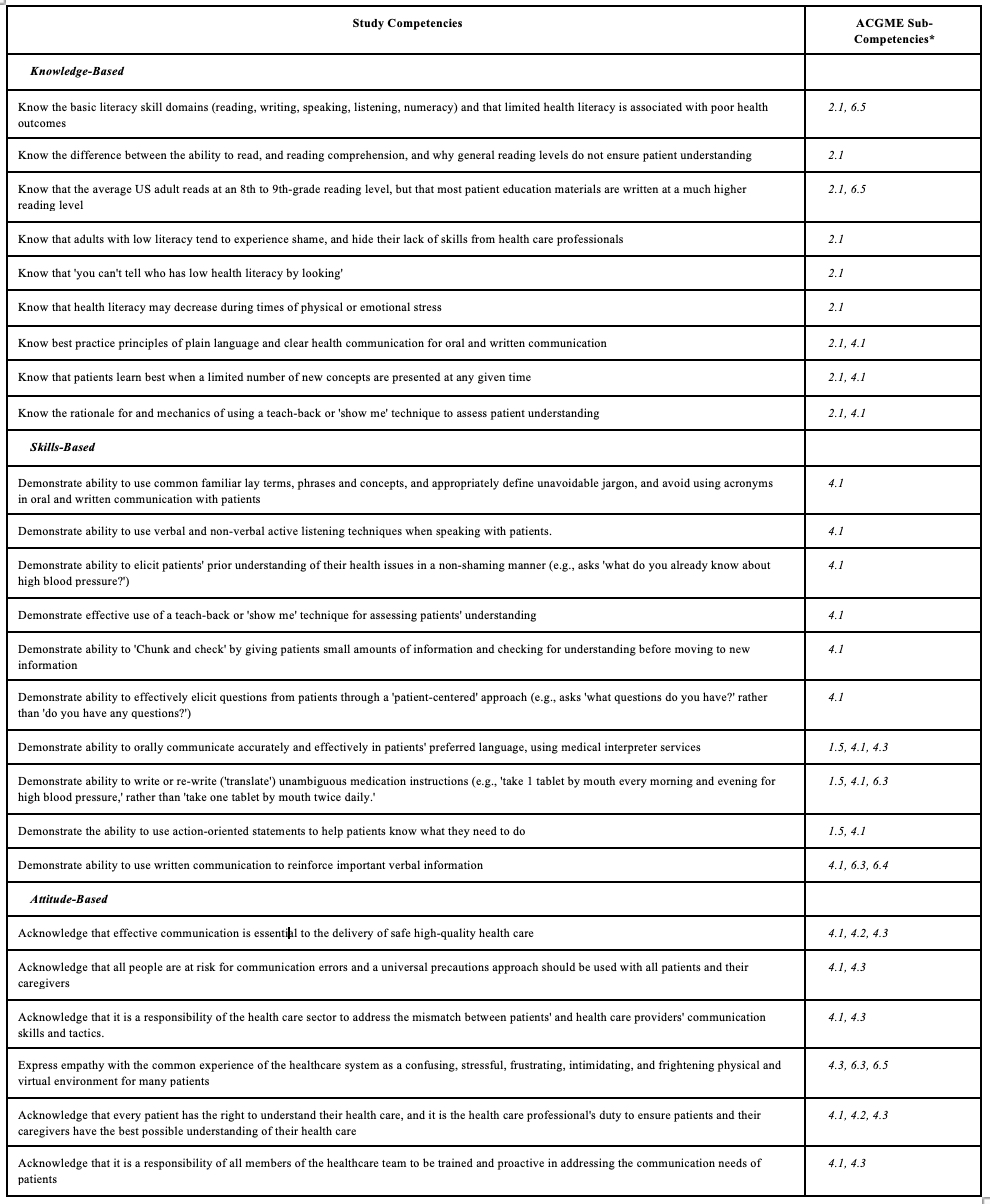
Results: Thirteen pediatric health literacy experts comprised a racially, geographically, and professionally-diverse panel (Table 1). There was no panelist attrition between the 2 rounds. Nine knowledge-based, 10 skills-based, and 6 attitude-based competencies met consensus after 2 rounds, several of which were re-worded based on panelist suggestions. Study authors mapped these competencies to relevant ACGME general pediatric sub-competencies, of which there were 8 (Table 2).
Conclusion(s): Through use of a pediatric lens, a panel of pediatric health literacy experts established consensus on health literacy-related competencies specifically for pediatric resident training. These prioritized knowledge, skills, and attitude items align with ACGME priorities, and provide more specific competencies to inform future health literacy curricula and assessment within pediatric residency programs.
.jpg)