Emergency Medicine: Quality Improvement
Emergency Medicine 5 B
339 - Implementation of an ED Nephrolithiasis Protocol Increases use of Medical Expulsive Therapy in the Pediatric Population
Publication Number: 339.209

Abhijeet S. Namjoshi, MD
Pediatric Resident
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background:
Despite the increase in nephrolithiasis in the pediatric population, many institutions do not have a standardized management pathway in the emergency department. A review of children presenting to our pediatric emergency department (PED) from 2011 to 2017 found that ureteral stone passage was significantly higher for those prescribed medical expulsive therapy (MET) versus analgesics alone (45% vs 20%, p< 0.0001). Urology consultation was also associated with increased MET use (p< 0.0001).
Objective:
To implement a nephrolithiasis management protocol at our PED, with goals of increasing MET usage, decreasing the use of computed tomography (CT) scans, and increasing outpatient referrals to Urology and Nephrology.
Design/Methods:
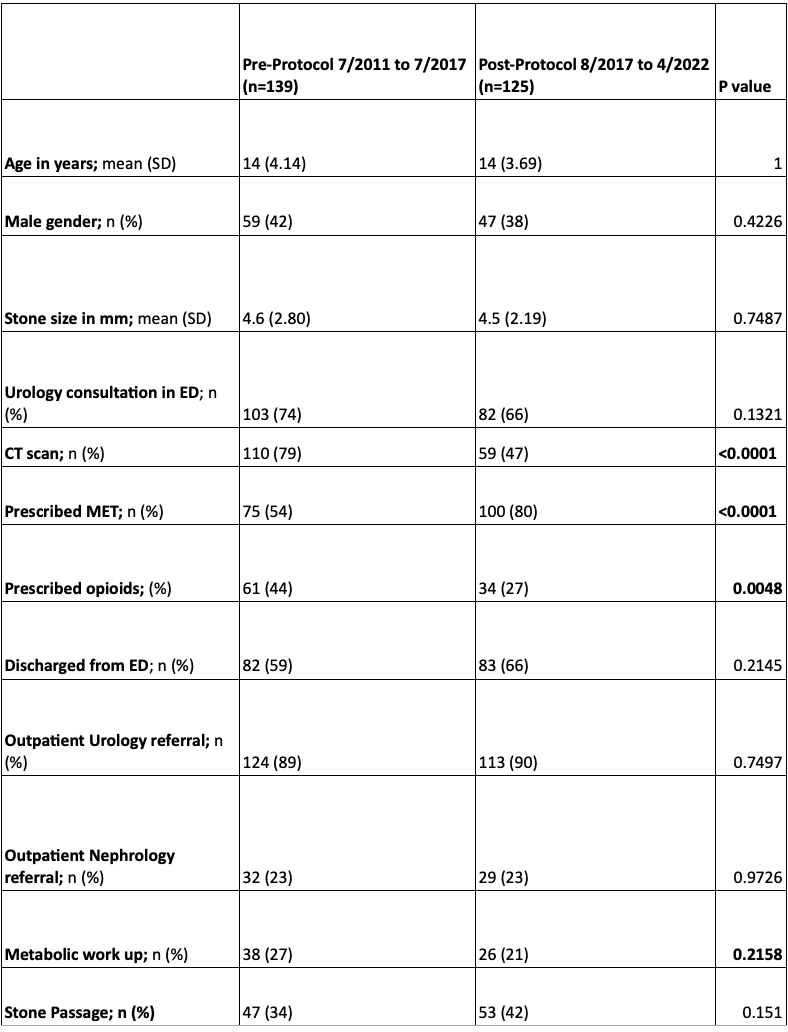
This is a retrospective study of children aged 2 months to 18 years old who presented to a quaternary PED with an ICD-9 or ICD-10 diagnosis of nephrolithiasis from August 2017 to April 2022. Basic demographic factors, MET prescribing, use of CT for stone diagnosis, opioid prescription rate, and referral to urology and nephrology were compared before and after implementation of the new PED nephrolithiasis protocol. Statistical analysis performed for age and stone size were done using two sided t-test. All other parameters analyzed using chi-squared (χ2) analysis.
Results:
125 patients met inclusion criteria. Mean age was 14 years (SD 3.69) with 47 male patients (38%). Compared to the 139 patients reviewed prior to protocol implementation, there was no significant difference in mean age, gender, stone size, discharge from ED, or urology consultation in ED between groups (Table 1). A total of 100 patients (80%) were prescribed MET, which was significantly higher compared with 54% prior to implementation of the protocol (p < 0.0001). Post protocol, 34 patients (27%) were prescribed opioids, which was significantly decreased compared with prior to protocol implementation (44%, p= 0.0048). There was significant decrease in the use of CT pre and post-protocol (79% vs. 47%, p < 0.0001). Urology was consulted in ED for 82 (66%) patients post-protocol, with 113 patients (90%) having outpatient urology referrals (p=0.7497). In comparison, 29 patients (23%) were referred to Nephrology. There was no significant difference in ED consultation or outpatient referrals compared with before protocol.
Conclusion(s):
After implementation of a PED nephrolithiasis protocol, use of MET for ureteral stones increased, prescribing of opioid medications decreased, and fewer CT scans were obtained. A dedicated and standardized pathway can improve care for the pediatric patient diagnosed with nephrolithiasis.