Emergency Medicine: Quality Improvement
Emergency Medicine 5 B
338 - Decreasing Unnecessary Point of Care Blood Glucose Testing (POCG) and Dextrose Boluses in the Pediatric Emergency Department (PED)
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 338
Publication Number: 338.209
Publication Number: 338.209
Saba Javadi, Cohen Children's Medical Center, Commack, NY, United States; Kimberly Kahne, Cohen Children's Medical Center, New Hyde Park, NY, United States; Amanda Leng Smith, Cohen Children's Medical Center, Plainview, NY, United States; Nehal J.. Shah, Cohen Children's Medical Center, New Hyde Park, NY, United States; Joshua Rocker, Cohen Children's Medical Center, New Hyde Park, NY, United States; Dana Libov, Department of Emergency Medicine Hofstra School of Medicine, Queens, NY, United States; Kim Giusto, Northwell Health, Rockville Centre, NY, United States

Saba Javadi, MD, MS (she/her/hers)
Resident Physician
Cohen Children's Medical Center
Commack, New York, United States
Presenting Author(s)
Background: There is a gap between current evidence-based management of hypoglycemia and the preferred practice at our institution. Since there is no standardized protocol, management is at the discretion of the provider, with variation amongst the medical team. This has led to dissemination of misinformation regarding hypoglycemia, adversely affecting patient care and causing overconsumption of hospital resources.
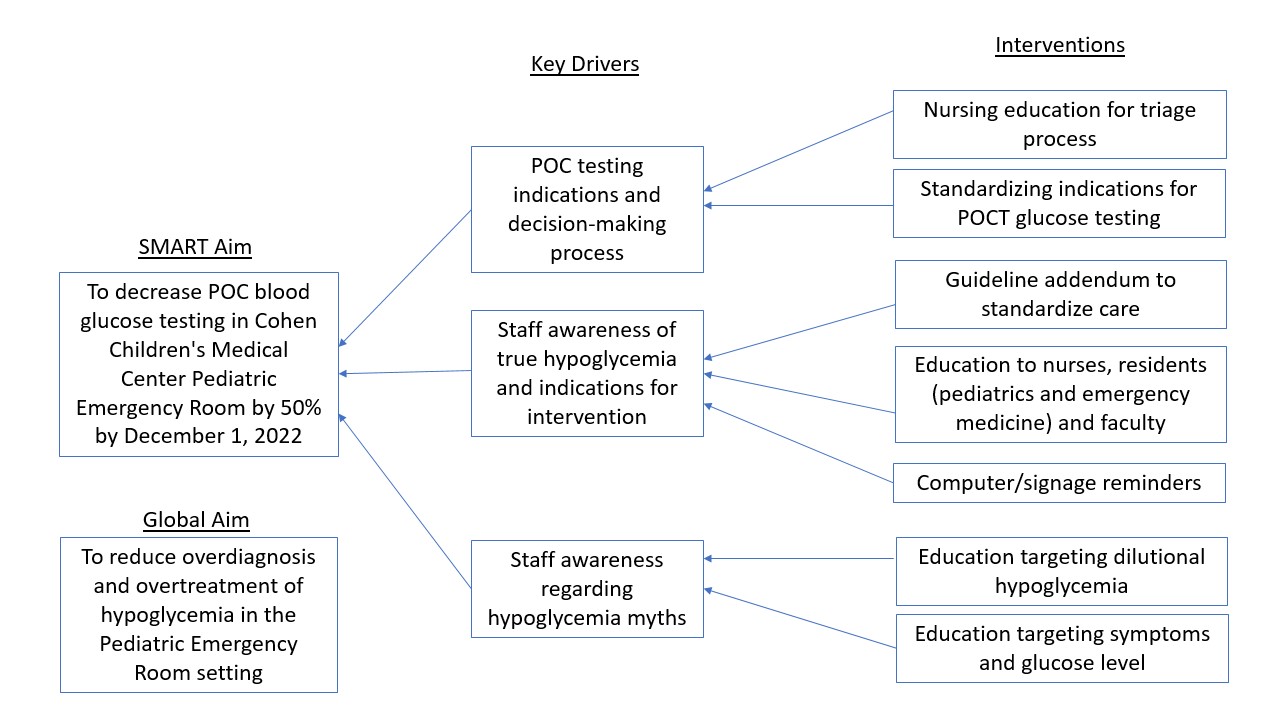
Objective: The objective of this study was to reduce the overdiagnosis and subsequent overtreatment of hypoglycemia, with the specific aim to decrease POCG testing in our PED by 50% by December 1, 2022.
Design/Methods: A multi-disciplinary team collaborated to create an algorithm for hypoglycemia management in the P</span>ED, using recommendations from the AAP, PES and WHO. A key driver (Fig. 1) was created to identify elements that contributed to the overdiagnosis and overtreatment of hypoglycemia. Interventions were implemented utilizing PDSA cycles from May 2022-August 2022. Data was obtained including POCG testing of total patient volume, dextrose 10% water bolus (D10W) administration of total patient volume, and D10W administration by POCG result. As a balancing measure, 72-hour returns admitted for dehydration over the intervention period were compared to the same months the year prior, to verify there was no increase. Data was plotted on run-charts to determine if there was special cause variation of shifts or trends that aligned with implementation of PDSA cycles.
Results: There was a significant decrease in POCG testing of total patient volume with three center line shifts in the desired direction (Fig. 2). There was also a decrease in overall D10W bolus administration during this time period with two center line shifts in the desired direction (Fig. 3). There was no decrease in D10W administration in patients with a known POCG 60-69 mg/dL. When compared to the same time period the year prior, there was no significant increase in patients returning to the PED requiring admission for dehydration (OR 1.11 [CI 0.69-1.69]).
Conclusion(s): POCG testing decreased by 50% of the amount prior to our interventions. The creation of an algorithm to standardize care led to a systemic change in management of hypoglycemia at our institution and will subsequently be used at other charter hospitals. Our interventions reduced the overall amount of dextrose boluses given, however it did not change the percentage of D10W boluses for POCG 60-69mg/dL. An official health-system-wide hypoglycemia guideline based on our algorithm is approaching publication, with the goal of improving upon these preliminary results.
.png)
.png)
