Hospital Medicine: Systems/Population-based Research
Hospital Medicine 4
505 - Hospital Discharge Services for Children with Medical Complexity: A Study of Children’s Hospitals
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 505
Publication Number: 505.221
Publication Number: 505.221
Yuliya Oumarbaeva-Malone, Children's National Health System, Washington, DC, United States; Valerie Jurgens, Children's National Health System, Alexandria, VA, United States; Margaret Rush, Childrens National Hospital, Washington, DC, United States; Miriam Bloom, Children's National Health System, Washington, DC, United States; Neha H. Shah, Children's National Hospital, Alexandria, VA, United States; Priti Bhansali, Children's National Health System, Washington, DC, United States; Kavita Parikh, Children's National Health System, Washington DC, DC, United States

Yuliya Oumarbaeva-Malone, MD (she/her/hers)
Pediatric Hospital Medicine Fellow PGY5
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background: Children with medical complexity (CMC) are increasingly cared for at children’s hospitals. This population of children are high healthcare utilizers and are at-risk for readmission after hospitalization. The full scope of programs and services to support hospital to home transitions for CMC is unknown.
Objective: We sought to describe the variety of discharge services provided to CMC at children’s hospitals in a national survey.
Design/Methods: We developed a survey to characterize availability of specific service lines and discharge services for CMC. A survey was electronically distributed to the 50 pediatric institutions within the Children's Hospital Association that contribute to the Pediatric Health Information Systems (PHIS). A 5-point Likert scale was used for frequency of discharge services. Responses were grouped: low frequency use (never and rarely), medium frequency use (sometimes), and high frequency use (most of the time and almost always).
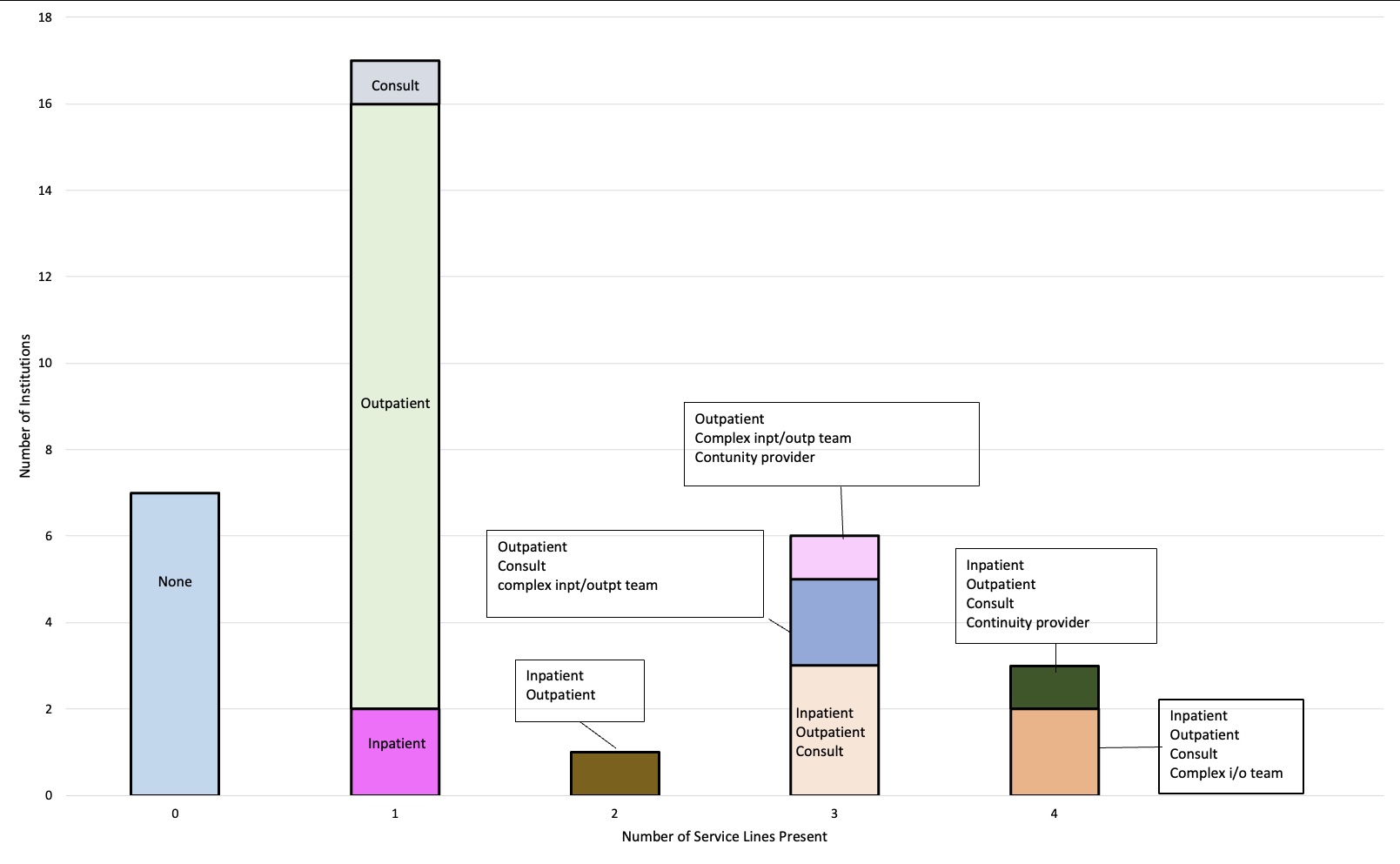
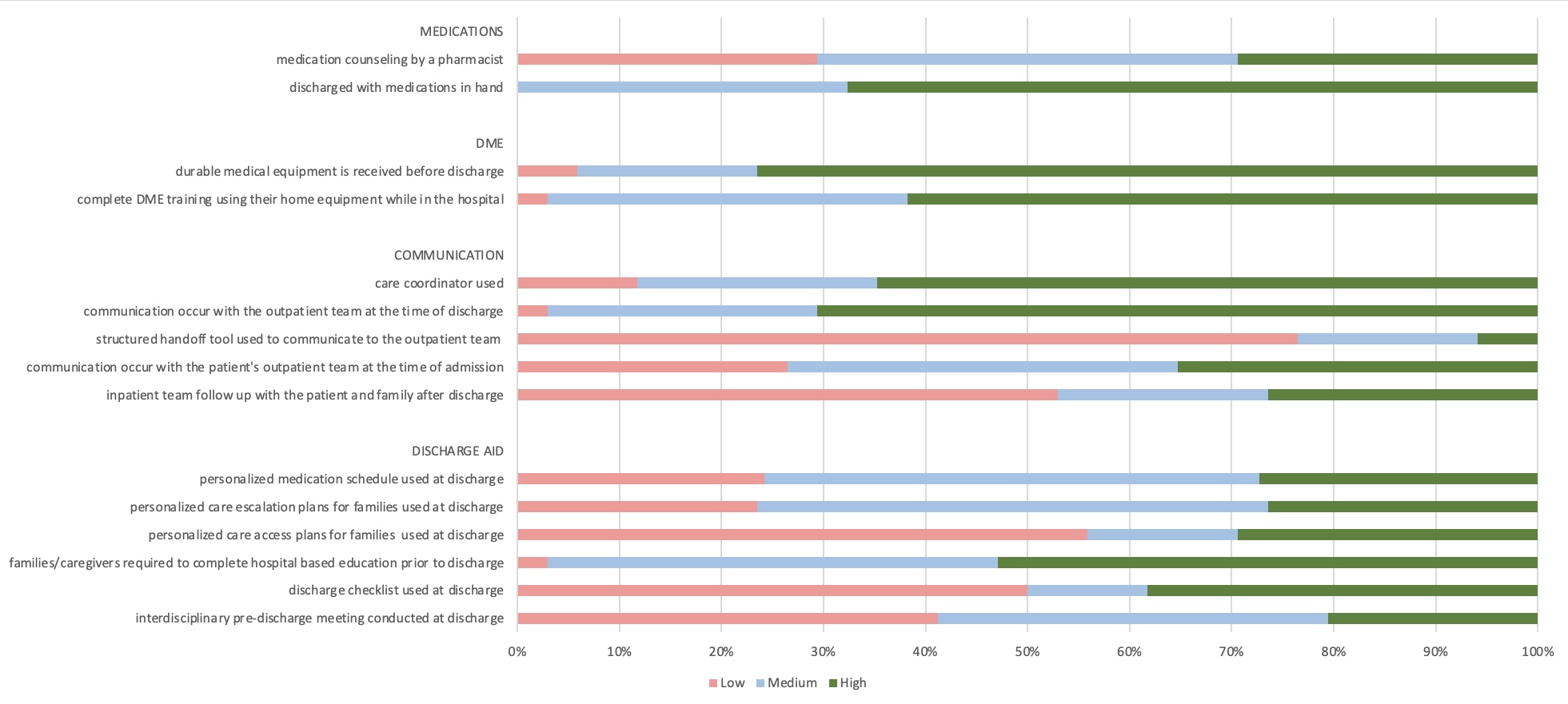
Results: 34 of 50 eligible hospitals responded to the survey (68% response rate). The majority have an outpatient care team (68%). Significant variety in care teams (Figure 1) and discharge services (Figure 2) was identified. Notably, medications in-hand at discharge was common (68%), though medication counseling by a pharmacist was not (29%). Most programs (76%) ensured durable medical equipment (DME) was delivered to the family prior to discharge, and ensured families were trained to use DME before discharge (62%). Communication with the patient’s outpatient provider was frequent (71%). Follow-up with the patient and their family by the inpatient team occurred less frequently (26%). Discharge aids were not commonly used, including personalized medication schedules (27%), individualized sick plans (26%), discharge checklists (39%), and discharge planning meetings (21%).
Conclusion(s): Children’s hospital services that support discharge of CMC vary significantly in structure and function. Future work will evaluate associations between care team structure and discharge services for CMC with healthcare utilization post-hospitalization.