Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 4
503 - Factors affecting admissions and readmissions in children with medical complexity
Publication Number: 503.221

Adam H. Rosenbloom, MD MPH (he/him/his)
Clinical Assistant Professor
University of Texas at Austin Dell Medical School
Austin, Texas, United States
Presenting Author(s)
Background:
Children with Medical Complexity (CMC) are a high risk population with a disproportionately high utilization of hospital services. This study adds to ongoing research that has aimed to provide a benchmark for hospitalization patterns in this population. This study focuses on a cohort at Children’s Comprehensive Care (CCC), a multidisciplinary primary care medical home located in Austin Texas that serves CMC.
Objective:
This retrospective study analyzes 5 years of hospitalization data to describe utilization patterns and illustrate risk factors that affect the frequency of admissions and readmissions.
Design/Methods:
The cohort of patients studied is defined by admission criteria to the CCC. These criteria are similar to previously published standard criteria for medical complexity. This study retrospectively analyzed these data using univariate and multivariate analysis.
Results:
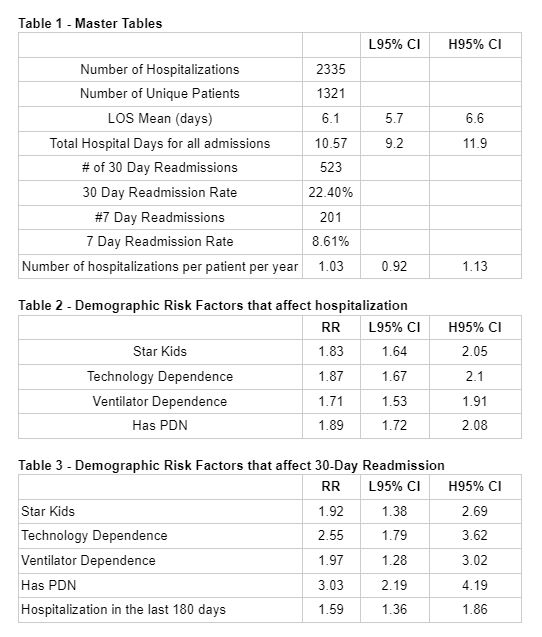
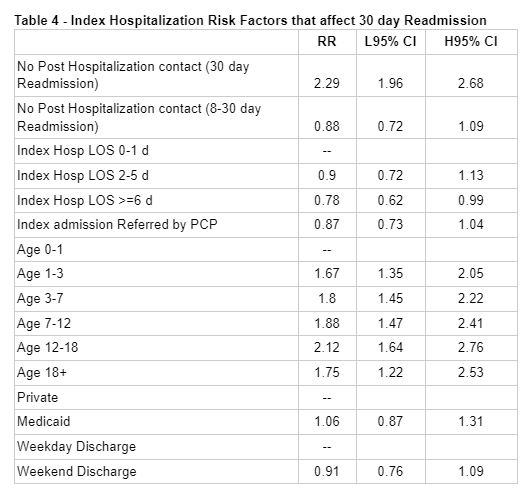
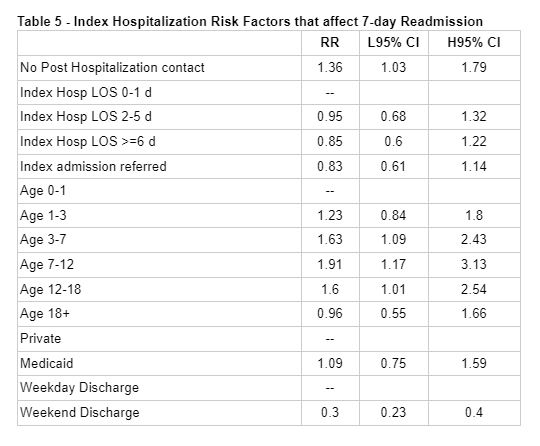
2335 hospitalizations, 523 30-day readmissions and 201 7-day readmissions were analyzed amongst 1321 unique patients. (Table 1) Demographic factors that increased the risk for any hospitalization were Medicaid status, Tracheostomy and Ventilator Dependence, and the presence of a Private Duty Nurse (PDN) in the home. (Table 2) Index hospitalization specific factors that increased the risk for 30-day readmission included Medicaid status, Tracheostomy and Ventilator Dependence, the presence of a PDN in the home, and hospitalization within the last 180 days. (Table 3) Increasing age increased the likelihood for 30-day readmission. An index hospitalization length of stay (LOS) of >6 days reduced the risk for 30-day readmission. Index hospitalization Private Insurance status, weekend discharge, and a post hospitalization follow up did not affect the risk for 30-day readmission. (Table 4) Index hospitalization specific factors that increased the risk for 7- day readmission included increasing age and no post hospitalization contact. A weekend discharge decreased the risk of a 7 day readmission. LOS and Medicaid Insurance did not affect the risk of a 7-day readmission. (Table 5) This study adds to the growing body of research for setting a benchmark for utilization patterns for CMC and building a predictive model for readmissions. What is new in this study is that this cohort is fully enrolled in a multidisciplinary primary complex care medical home. Most of the risk factors identified reflect a level of medical complexity, a non-modifiable variable. This study can inform further QI initiatives to prevent unnecessary readmissions while recognizing the non-modifiable natural history utilization patterns of CMC.
Conclusion(s):