Developmental and Behavioral Pediatrics: Screening & Assessment
Developmental and Behavioral Pediatrics 3
408 - Psychometrist Financial Model for a Developmental and Behavioral Pediatric Academic Practice
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 408
Publication Number: 408.206
Publication Number: 408.206
Medha Desai, University of Louisville School of Medicine, Louisville, KY, United States; Christian Flynn, University of Louisville School of Medicine, Louisville, KY, United States; Alisha Deshmukh, University of Louisville School of Medicine, Louisville, KY, United States; Luke T. Byerly, University of Louisville School of Medicine, Louisville, KY, United States; Thomas Beyerle, University of Louisville School of Medicine, Pewee Valley, KY, United States; Maria Romelinda L. Mendoza, University of Louisville School of Medicine, Louisville, KY, United States; Beth Spurlin, University of Louisville, Louisville, KY, United States; In Kim, University of Louisville School of Medicine, Louisville, KY, United States
Medha Desai, BS (she/her/hers)
Medical Student
University of Louisville School of Medicine
Louisville, Kentucky, United States
Presenting Author(s)
Background: The current national average wait time for an initial consult for developmental and behavioral disorders is 12-15 months. In some US regions, the wait time can be greater than 24 month. Often, there are not enough Developmental Behavioral Pediatricians (DBP) to fulfill this high demand for evaluations.
Objective: To address this high demand, a cost-effective analysis was performed for utilizing a psychometrist in a DBP practice which may help reduce current wait times by increasing throughput.
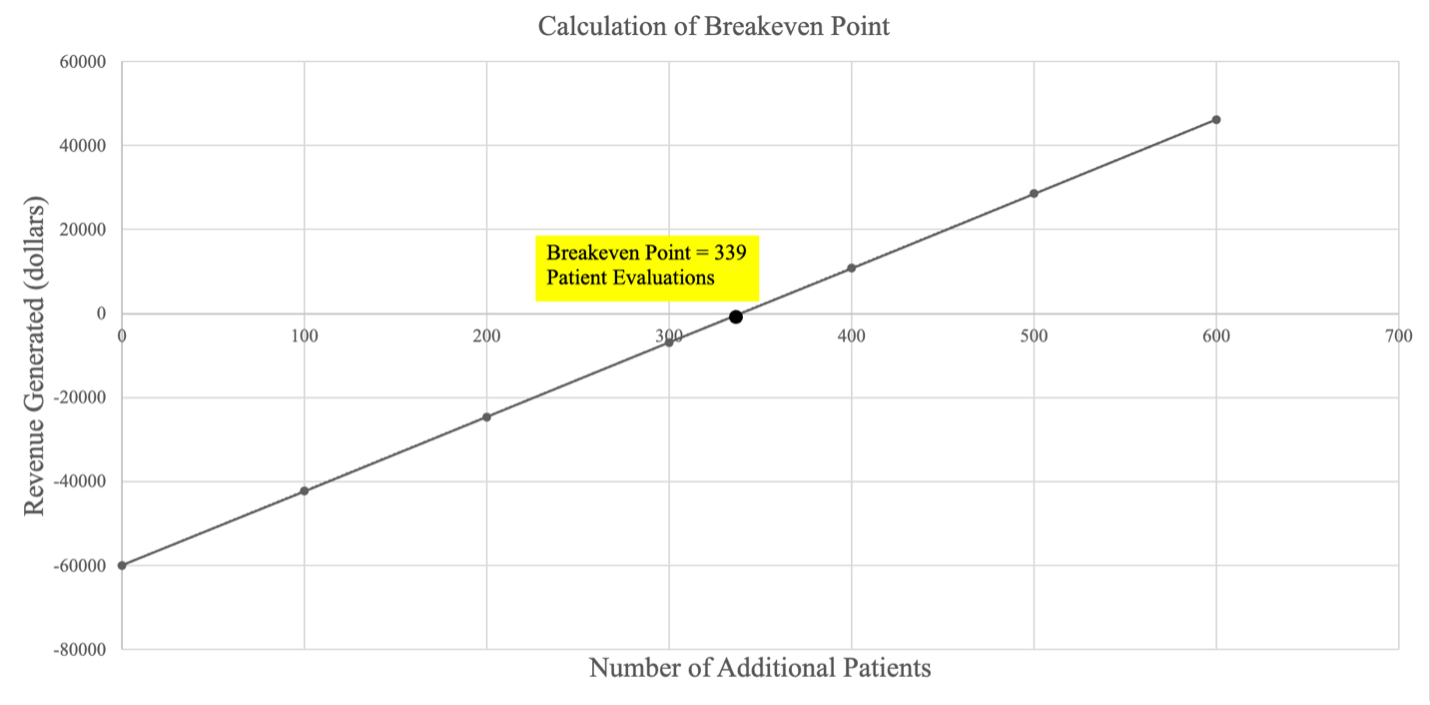
Design/Methods: Initially, Medicaid billing codes for psychometrists were obtained for the financial model. Patient throughput at Norton Children’s Development Center (NCDC) was used to model how an additional psychometrist would impact patient throughput and DBP scheduling. Finally, this model was used to evaluate the estimated additional revenue generated by NCDC with the addition of one psychometrist. Total revenue and total expenses were calculated as well as net revenue. A breakeven point was calculated for hiring an additional psychometrist.
Results: By hiring one psychometrist, approximately 1,536 additional hours annually are generated for DBPs. This additional time could be used to generate additional revenue with more visits or longer visits. Total Revenue for one year was $272,087. Total expenses were $60,000. Net revenue generation was $212,087 from one psychometrist. The breakeven point was calculated to be 339 patients annually.
Conclusion(s): Our financial model illustrates that the addition of a psychometrist may be clinically and financially advantageous. The utilization of a psychometrist generates additional revenue while concomitantly may improve patient throughput. By utilizing a psychometrist, we may have a cost effective solution to address prolonged wait times for DBP patients.
.png)
