Medical Education: Faculty Development
Medical Education 5: Faculty Development 1
521 - Pediatric Emergency Physician Self Efficacy of Emergent Procedures after a Cadaveric Porcine Skills Maintenance Lab
Publication Number: 521.227
Andrew S. Oh, MD
Fellow
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background:
Critical life-saving procedures are rarely performed on children among large, free-standing pediatric Emergency Departments or combined Level 1 adult/pediatric trauma centers. Methods to sustain competence of low volume, high-risk procedures among Pediatric Emergency Medicine (PEM) physicians are needed. Cadaveric porcine models provide minimal cost (approximately $115 per person) and administrative burden but the impact on proceduralist self-efficacy is not known.
Objective:
To assess the change in self-efficacy among PEM physicians after participation in a cadaveric porcine skills lab designed to train on critical life-saving procedures.
Design/Methods:
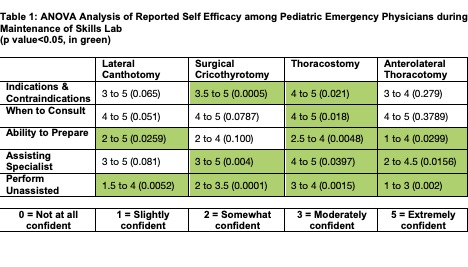
PEM physicians and post-graduate fellows participated in a 4-hour cadaveric porcine skills lab designed to train on four procedural skills: lateral canthotomy (LC), surgical cricothyrotomy (SC), tube thoracostomy (TT), anterolateral thoracotomy (AT). Levels of participant self-efficacy were assessed before and after participation in the lab using a 5-point Likert scale (1 = not at all confident to 5 = extremely confident) across five categories of proper execution: procedure indications/contraindications, preparation and set up, indications for subspecialist consultation, assisting the subspecialist during the procedures, and unassisted performance of the procedures. Change in self-efficacy was assessed using within-subject Analysis of Variance (ANOVA). Perception of relevance and necessity to clinical practice for the 4 procedures were assessed using a 7-point Likert scale.
Results:
A total of 20 PEM physicians participated in the skills lab. There was a statistically significance increase in self-efficacy related to unassisted performance of all 4 procedures: LC (1.5 to 5, p< 0.005), SC (2 to 3.5, p< 0.0001), TT (3 to 4, p< 0.001), AT (1 to 3, p< 0.002). Self-efficacy increased for assisting the specialist in 3 of the 4 procedures: SC (3 to 5, p< 0.004), TT (4 to 5, p< 0.039), AT (2 to 4.5, p< 0.015). Tube thoracostomy had significance in all five categories of proper execution (Table 1). Participants strongly agreed that competence in skill performance was highly relevant (median 7, IQR 6, 7) and highly necessary (median 7, IQR 6, 7) in their clinical practice.
Conclusion(s):
Participation in a cadaveric porcine skills lab resulted in increases in self efficacy for four emergency procedures among PEM physicians. Further studies should assess competency of providers trained in this manner.