Medical Education: Simulation & Technology
Medical Education 6: Simulation & Technology 1
529 - Evaluation of a Novel Simulation Rotation for Pediatric Residents to Teach Crisis Resource Management Skills
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 529
Publication Number: 529.228
Publication Number: 529.228
Lorel Huber, University of Colorado School of Medicine, Aurora, CO, United States; Robert Bishop, University of Colorado School of Medicine, Aurora, CO, United States; Shannon Flood, Children's Hospital Colorado, Denver, CO, United States; Ryan Good, University of Colorado School of Medicine, Aurora, CO, United States; Christopher S.. Nichols, University of Colorado School of Medicine, Aurora, CO, United States; Kathryn A. Walsh, Denver Health / University of Colorado / Children's Hospital Colorado, Denver, CO, United States

Lorel Huber, MD (she/her/hers)
Fellow Physician
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: Pediatric residents lack the knowledge and hands-on practice required to be competent leaders at resuscitations and code events. To evaluate this known educational gap, we conducted a local needs assessment and found that our pediatric residents have little resuscitation experience and do not feel confident leading resuscitations.
Objective: To develop a simulation-based rotation for pediatric residents to improve capability and confidence in crisis resource management skills including leadership, airway and breathing support, circulation and arrhythmia management.
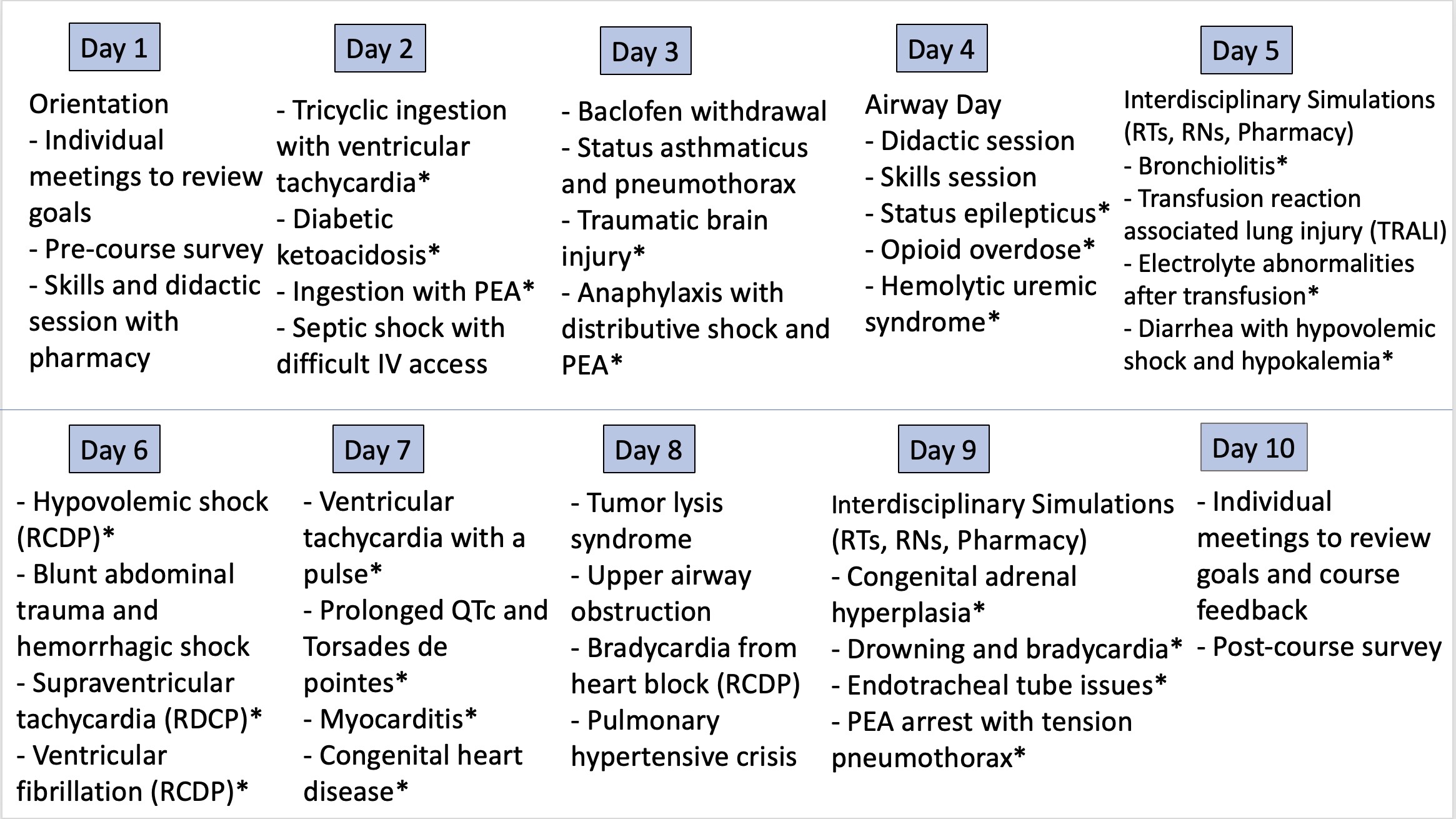
Design/Methods: Using Kern's six steps of curriculum development, we designed a 10-day rotation for 2nd and 3rd year pediatric residents that included 31 high-fidelity simulations (Figure 1). Other teaching modalities included skills trainers, didactic sessions and self-directed learning. The course content was developed using Pediatric Advanced Life Support (PALS) materials and gaps identified in the needs assessment. Detailed learning objectives and a topic checklist were created. Course facilitators developed most simulations, and some were adapted from previously publications.
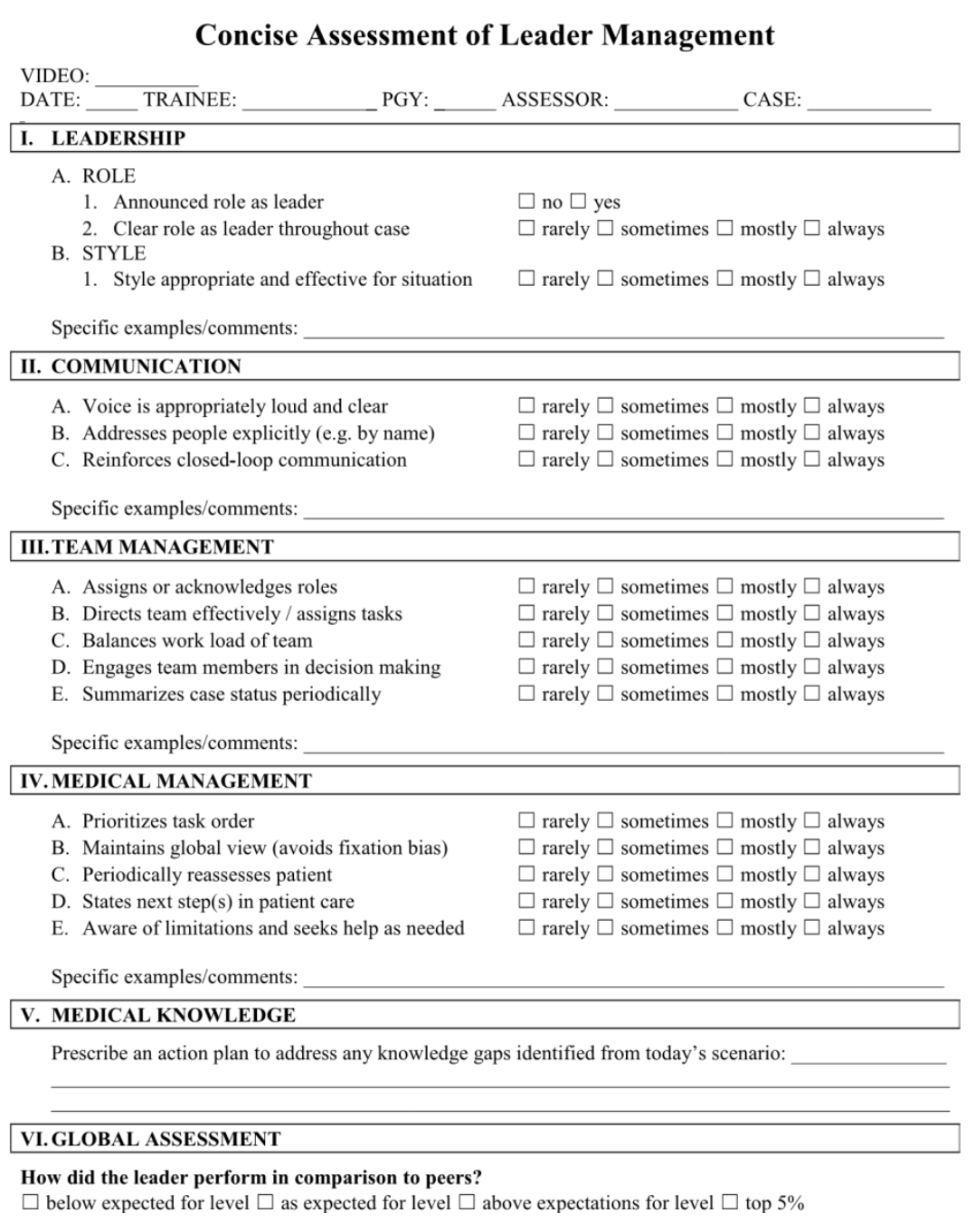
We evaluated the curriculum using the Concise Assessment of Leader Management (CALM) instrument which evaluates leadership, communication, team management, and medical management (Figure 2). We scored residents leading their first and last simulation using the CALM tool. Residents also completed a pre- and post-course survey that included a five-point Likert scale for self-perceived confidence and capability when approaching a patient needing resuscitation.
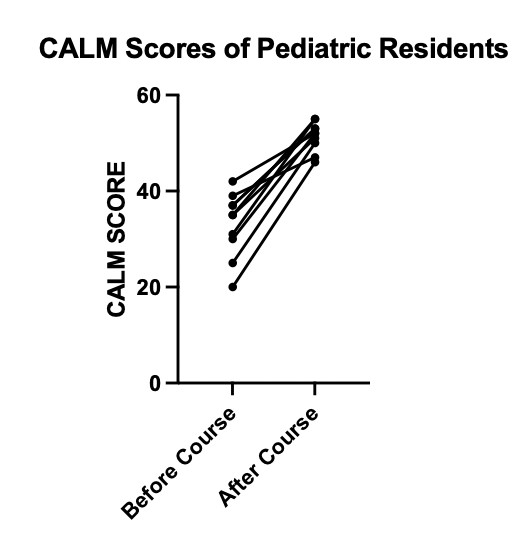
Results: Among the 25 residents who have completed the simulation rotation, 10 were evaluated using the CALM tool, and 17 completed the pre/post survey. There was significant improvement in the CALM score on the residents' last simulation as compared to their first simulation (median 52 vs 35, p-value < 0.002, n=10; Figure 3) indicating improvement in leadership ability at the end of the course. Residents also reported significant improvement in self-perceived confidence (median 2 vs 4, p-value < 0.0002, n=17) and capability (median 2 vs 4, p-value < 0.0001, n=17) when approaching a patient needing resuscitation before and after the course.
Conclusion(s): We developed a simulation-based rotation for pediatric residents that improved leadership skills and resident self-perceived levels of capability and confidence when approaching a patient resuscitation. Future work should focus on assessment of competency and retention of resuscitation skills learned in this course.