Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 5
448 - Perceptions of a Clinical Program to Address Menstrual Poverty: A Mixed Methods Study
Publication Number: 448.219

Natalie Wichelt, MD/MPH (she/her/hers)
Pediatric Resident
Atrium Health Wake Forest Baptist
Winston Salem, North Carolina, United States
Presenting Author(s)
Background:
Menstrual poverty, inadequate access to menstrual hygiene tools, has been associated with emotional well-being, school attendance, and health autonomy. However, little research exists assessing a pediatric clinical program addressing menstrual poverty.
Objective:
This mixed methods study aimed to examine how menstrual poverty can be addressed in a clinical setting through screening and access to menstrual products. It also explored patient and provider perceptions of the clinical program.
Design/Methods:
We introduced a novel screener in April 2022 at one academic pediatric clinic. We partnered with a local organization, The Homeless Period Project, to create packets containing menstrual supplies. A survey was provided at each menstruating adolescent well child check and patients were asked: In the last 12 month, (1) have you needed period products but not had enough money to buy them? (2) have you missed school because you did not have enough period projects? (3) have you ever felt stressed about your periods due to not having enough period products? We analyzed 73 completed surveys from 4/20/22 to 7/20/22 using descriptive statistics. A “yes” answer to at least one question was considered a positive screen. Those with positive screens were given the option of receiving a menstrual supply packet and invited to participate in semi-structured phone interviews. Clinic providers also participated in semi-structured interviews. Interviews were recorded, transcribed, verified against the audio and analyzed using thematic analysis.
Results:
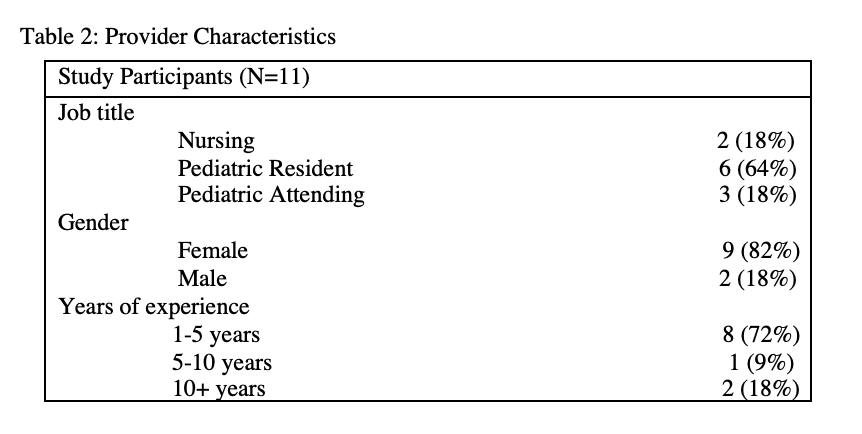
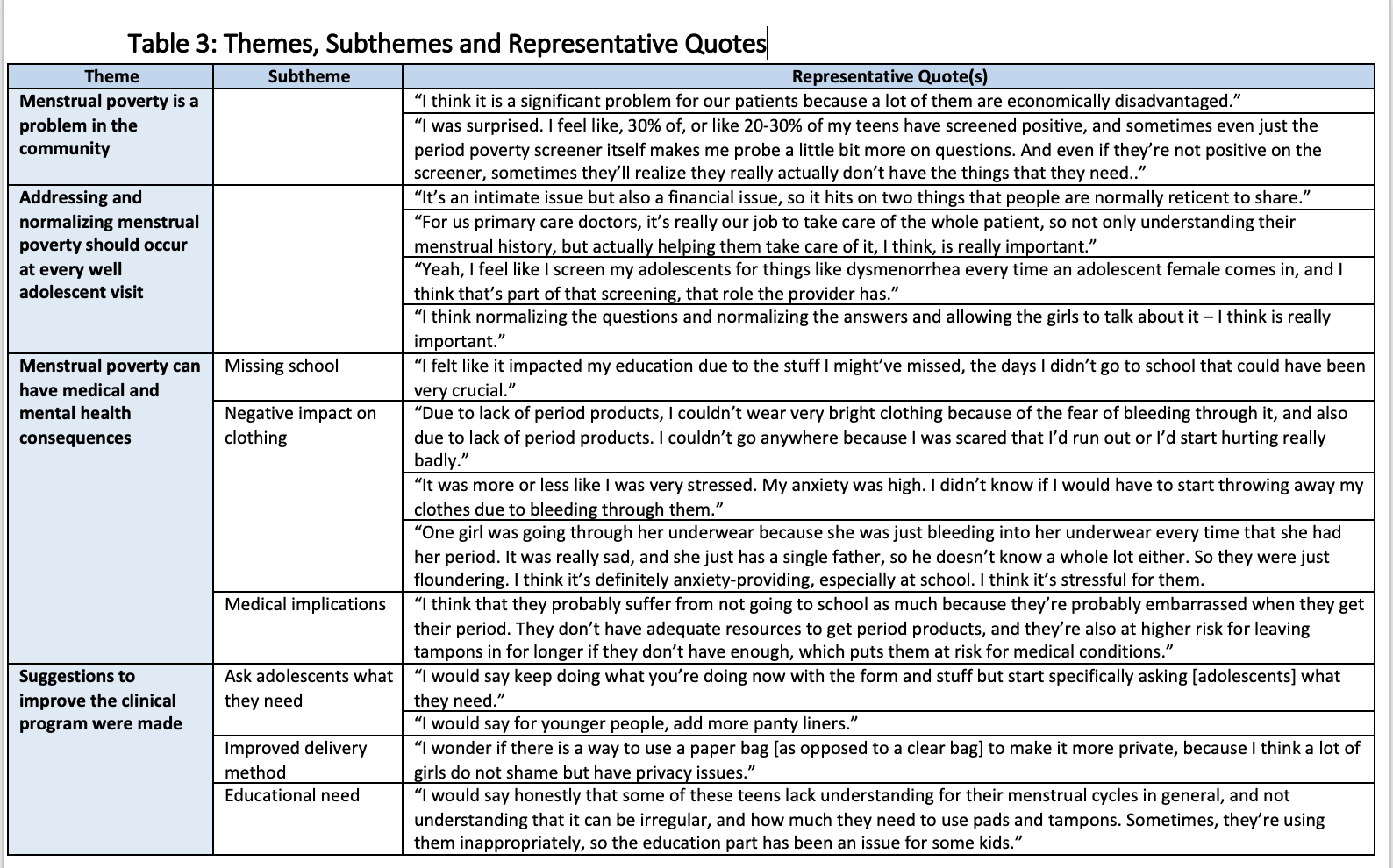
Of the 73 completed surveys, 10% were positive for at least one question; 10% reported needing period products; 7.1% reported missing school; 10% felt stressed about their periods. Of the 11 participants who screened positive, 7 completed semi-structured interviews (Table 1). Additionally, 11 pediatric providers were interviewed (Table 2). Themes included: (1) menstrual poverty is a problem in the community, (2) addressing and normalizing menstrual poverty should occur at every adolescent well visit, (3) menstrual poverty can have medical and mental health consequences, and (4) suggestions to improve the clinical program (Table 3).
Conclusion(s):
We found that a clinical program addressing menstrual poverty was acceptable among patients and providers. Additional research is needed to determine effectiveness..png)