Mental Health
Mental Health 2
394 - Leveraging the Electronic Health Record to Improve Evidence Based Care for Anxiety and Depression
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 394
Publication Number: 394.231
Publication Number: 394.231
Michael Kantor, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Sandra H. Jee, Golisano Children's Hospital at The University of Rochester Medical Center, Rochester, NY, United States; Cynthia Rand, University of Rochester, Golisano Children's Hospital, Rochester, NY, United States; Andrew Cohen, Pediatric Practice at Golisano Children's Hospital, Rochester, NY, United States

Michael Kantor, MD (he/him/his)
General Academic Pediatric Fellow
University of Rochester School of Medicine and Dentistry
Rochester, New York, United States
Presenting Author(s)
Background: Anxiety and depression are adding to the burden of chronic illness and healthcare
utilization in pediatric populations, particularly during and after the COVID-19 pandemic. The
literature shows that despite increases in the prevalence of mental health disorders, the majority
of patients do not receive physician-directed care for these conditions, especially those living in
poverty.
Objective: To use quality improvement (QI) methods to increase providers’ adherence to
professional organizations’ guidelines for anxiety and depression in an urban academic practice
clinic that professional organizations endorse. We aimed to increase the proportion of the
proportion of clinical encounters in which recommended management was addressed by 20% in
12 months.
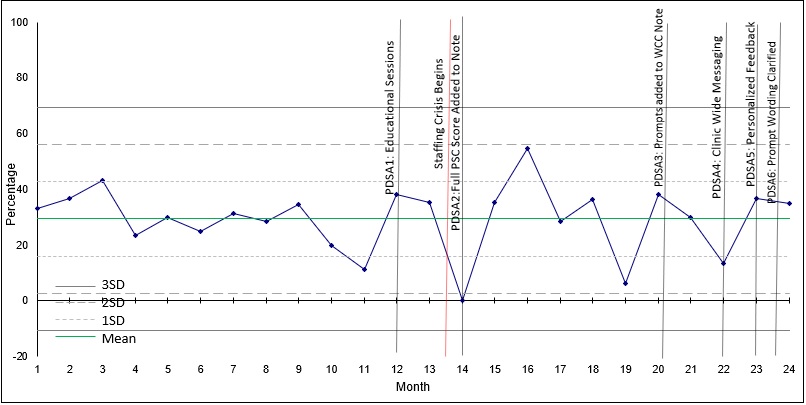
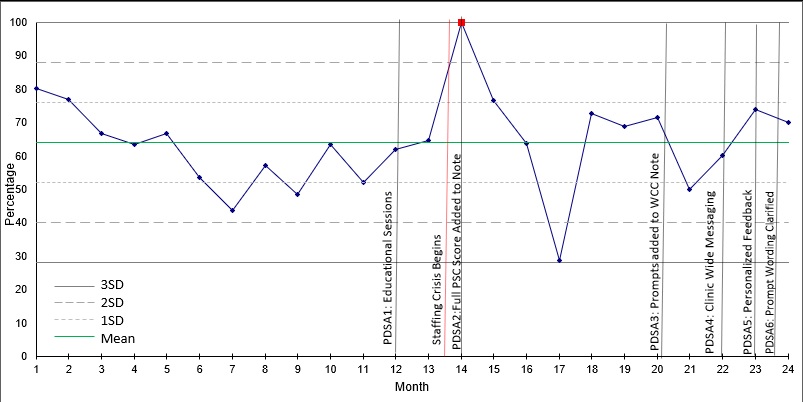
Design/Methods: The QI intervention included 1) an educational session for providers on screening and management 2) changes to EHR note templates, and 3) personalized feedback to providers. Over 6 PDSA
cycles, providers received EHR prompts to address 1) guideline-based diagnosis, 2) behavioral
health referral, 3) discussion of medication, and 4) follow-up for depression and anxiety
symptoms. We aimed to review charts of 30 patients who had screened positive on the internalizing
domain of the Pediatric Symptom Checklist-17 each month. We assessed whether the 4 areas of
recommended guidance had been addressed. Data were analyzed on statistical process control
charts (SPC), and outcome means were compared for significant differences using the Mann-
Whitney U test.
Results: We reviewed 329 encounters over the 12-month baseline and 205 encounters over the
12-months intervention period. The median rate of adding a mental
health diagnosis to the problem list rose from 55.2% preintervention to 58.8% post-
intervention (p=.795). The median rate of referral discussion rose from 63.3% to 68.8%
(p=.194). The rates of medication discussion fell from 36.7% to 33.3% (p=.982). Rates of
follow-up rose from 30% to 35.3% (p=.689). No measured outcomes met criteria for
special cause variation on the SPC charts (Figs 1-3). A staffing crisis was experienced during this
time and noted on the SPC.
Conclusion(s): An educational intervention, EMR template changes, and personalized feedback did
not significantly affect providers’ rates of adherence to guidelines for managing anxiety
and depression. These findings may be attributable to the challenge of introducing new activities
into a busy practice during staff turnover and shortages. Next steps will be to explore
barriers with providers, staff, and patients to improve outcomes for patients with mental health
conditions.
.jpg)