Medical Education: Simulation & Technology
Medical Education 6: Simulation & Technology 1
528 - Advancing Recognition of Resuscitation Medication Location in Emergencies (ADRENALINE): A Quality Improvement Initiative in Nursing Education Using Deliberate Practice Simulation
Publication Number: 528.228

Natalie J. Tedford, MD (she/her/hers)
Pediatric Emergency Medicine & Global Health Fellow
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background:
Timely medication intervention in patient codes and acute resuscitations is crucial for optimal patient outcomes. Deliberate practice simulation (DPS) is a tool that can enhance learning through repetitive, task-oriented education with immediate feedback and serve as a mechanism to address nurses’ unfamiliarity with location of crucial medications in emergency settings.
Objective:
To increase nurses’ knowledge and accurate location identification of commonly used medications in emergency settings.
Design/Methods:
We initiated an educational, quality improvement project designed for nurses working in the pediatric emergency department at a level 1 pediatric trauma center. We collected quantitative needs assessment then baseline data regarding nurses’ knowledge of acute/code medications’ location (i.e., crash cart, automated-drug-dispensing-cabinet, pharmacy). PASS was considered 26 out of 33 correct on graded electronic surveys. Three plan-do-study-act (PDSA) cycles (see Figure 1 for timeline). Education was provided via monthly newsletter medication highlights bundled with 3-question quizzes and DPS with use of the crash cart and verbal quizzing on the medications. Data were analyzed using descriptive statistics, and paired t-tests were conducted to determine the effect of DPS on nurses’ PASS rates on our graded electronic surveys.
Results:
There were 36 nurses who participated with majority (86%) routinely working in the emergency department. With use of DPS, there was a notable increase the percentage of nurses who achieved “PASS” from 8% (mean=21.2, SD=3.2, n=36) to 64% (mean=25.9, SD=2.6, n=36), see Figure 2. Between PDSA cycles 1 and 2, correct location identified increased from 69% to 77%, revealing overall improvement on paired sample t-test (mean increase of 8%, p< 0.003) (Table 1). Participants demonstrated an improvement on paired sample t-test in knowledge assessment scores (mean increase of 4.6 points or 22%, p < 0.00001).
Conclusion(s):
Our education-directed quality improvement initiative demonstrates notable improvement in nurse knowledge of resuscitation medication location in emergencies through use of deliberate practice simulation. Our efforts show promise in advancing efficiency in patient resuscitations and provide opportunities for improvement through iterative PDSA cycles. Next steps will be to link clinical outcomes.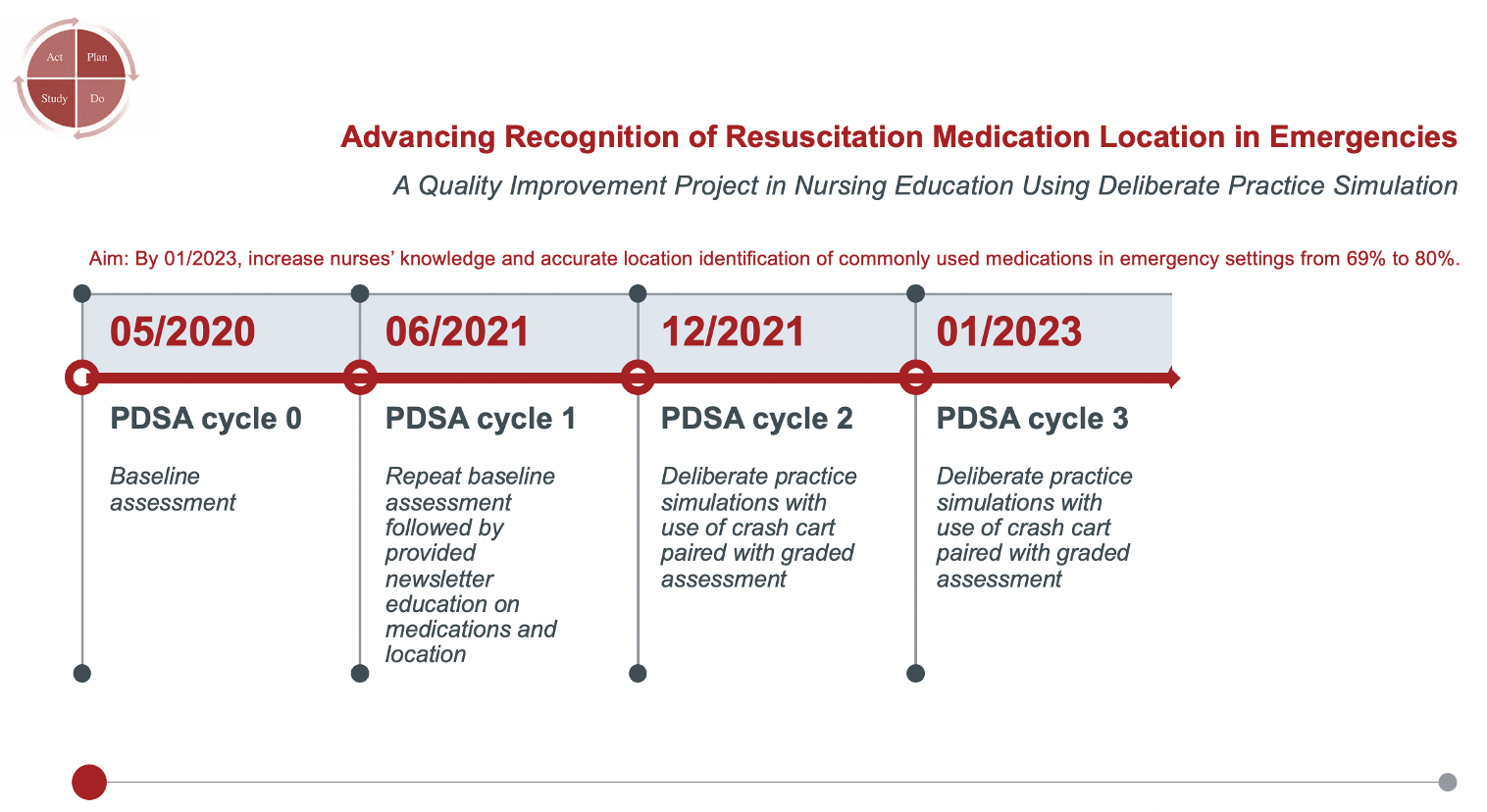
.png)
.png)
