Emergency Medicine: Quality Improvement
Emergency Medicine 5 B
345 - Pediatric Ovarian Torsion Evaluation in the Emergency Department: A Quality Improvement Initiative
Publication Number: 345.209

Brian L. Park, MD (he/him/his)
Pediatric Emergency Medicine Fellow
University of Washington School of Medicine
Seattle, Washington, United States- SF
Presenting Author(s)
Co-Author(s)
Background: Transabdominal pelvic ultrasound (TPUS) is the diagnostic test of choice when evaluating for ovarian torsion, a time-sensitive surgical emergency, in pediatric patients presenting to the emergency department (ED), and requires a full bladder to adequately visualize the ovaries. Prior to this quality improvement (QI) initiative, the bladder filling process at our institution was not standardized and varied by provider, resulting in long wait times to TPUS, inadequate visualization of ovaries requiring repeat studies, and prolonged emergency department length-of-stay (ED LOS).
Objective:
The primary objective was to decrease the monthly mean time to TPUS by 20 minutes over a 1-year period through standardization of the bladder filling process in patients being evaluated for ovarian pathologies with TPUS.
Design/Methods:
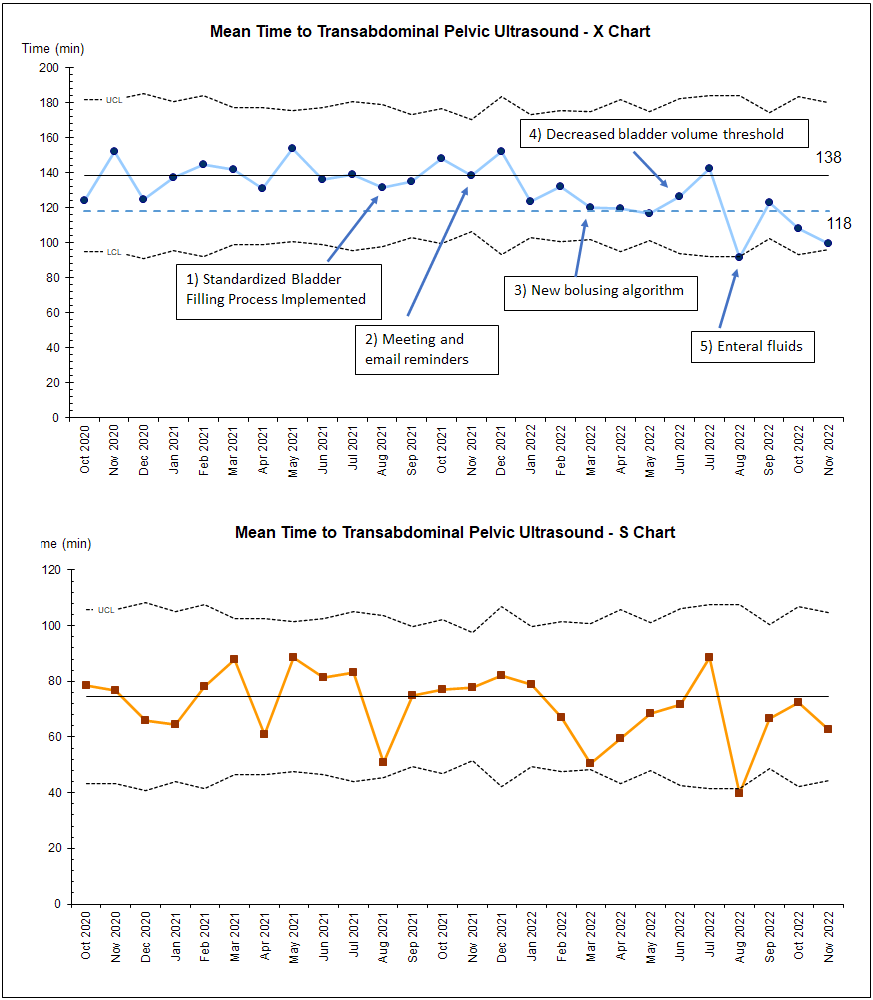
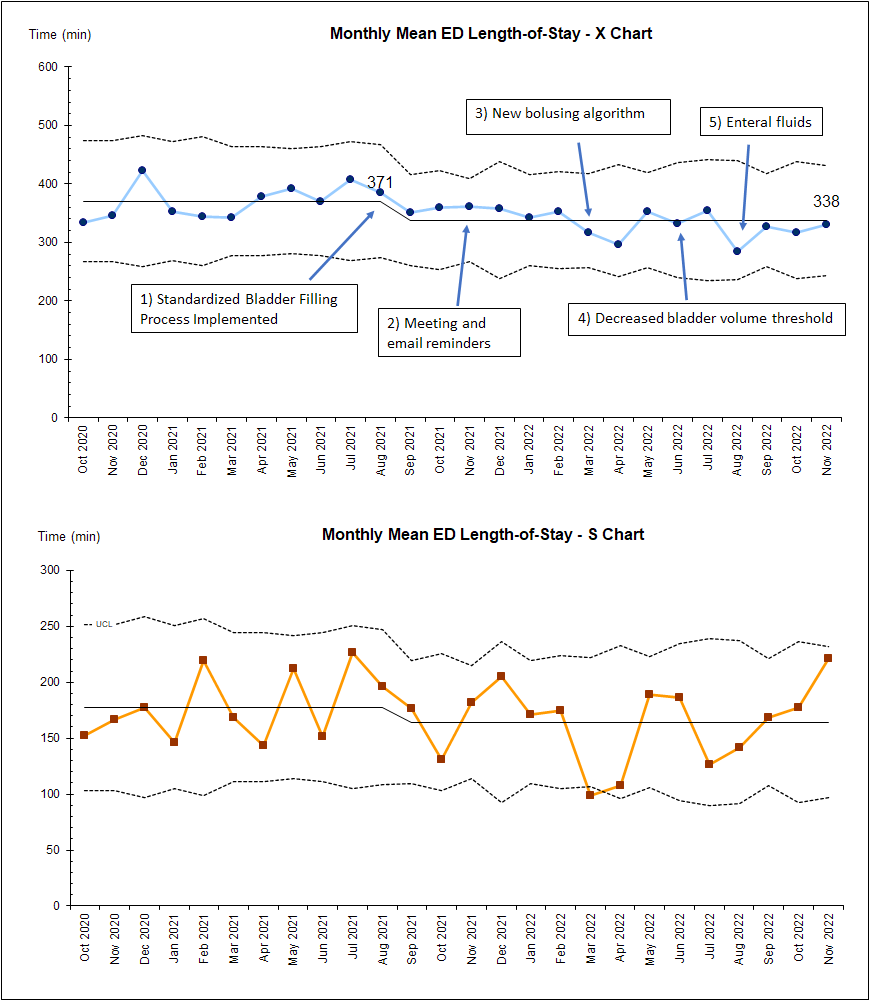
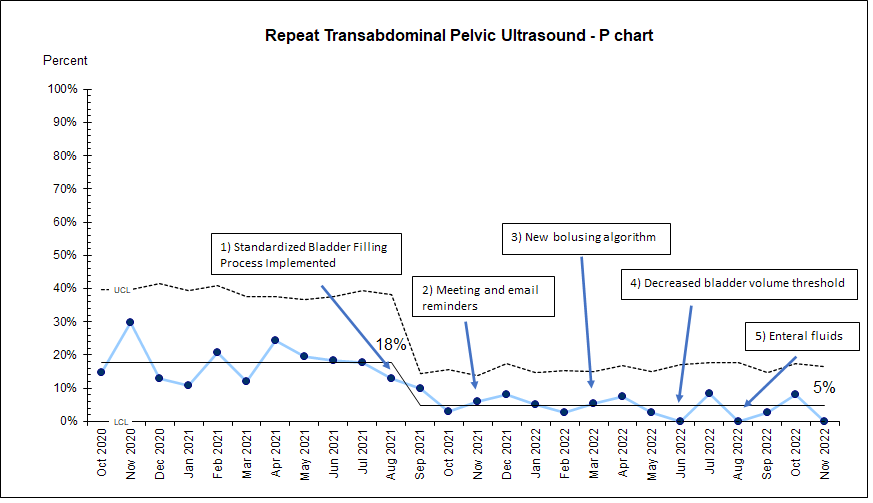
This was a QI initiative at a single, academic, quaternary-care children’s hospital ED. We utilized the Institute for Healthcare Improvement Model for Improvement with sequential Plan-Do-Study-Act (PDSA) cycles. First interventions were implemented in August 2021 and included a new electronic order set, bedside bladder scan by ED nurses, and rapid delivery of intravenous (IV) fluids. Subsequent interventions aimed to decrease time to IV fluid, decrease fluid requirement, and decrease need for IV fluid. The primary outcome measure was monthly mean time to TPUS. Secondary outcome measures were monthly mean ED LOS and percentage of repeat TPUS due to inadequate visualization of ovaries. Data were analyzed with statistical process control charts to assess for system change over time.
Results:
292 ED encounters over 10 months were used to establish pre-intervention baseline, and 526 ED encounters over 16 months were reviewed post-intervention. The baseline mean time to TPUS and ED LOS were 138 minutes and 371 minutes, respectively. 18% of patients required repeat TPUS prior to intervention. Both time to TPUS and ED LOS showed improving trend, but only ED LOS met special cause variation with improvement of 33 minutes (Figure 1&2). Percentage of repeat TPUS decreased to 5% with special cause variation (Figure 2).
Conclusion(s):
Time to TPUS showed an improving trend without meeting special cause variation after standardization of bladder filling process. ED LOS demonstrated improvement that appears to correlate with decreasing time to TPUS and repeat studies. Assessment of bladder fullness with bladder scan prior to TPUS decreased the need for repeat studies. Challenges in improving time to TPUS may include increasing ED patient volume and staffing challenges in the ED during the study period.