Emergency Medicine: All Areas
Emergency Medicine 7
367 - The Effect of Step Stool Use on Chest Compression Quality During CPR in Young Children: Findings from the Videography in Pediatric Emergency Research (VIPER) Collaborative
Publication Number: 367.211
- KO
Karen O'Connell, MD, MEd (she/her/hers)
Professor of Pediatrics and Emergency Medicine
Children's National Hospital
The George Washington University of Medicine and Health Sciences
Washington, District of Columbia, United States
Presenting Author(s)
Background:
Delivering chest compressions (CC) of adequate depth and rate during pediatric cardiopulmonary resuscitation (CPR) has known beneficial hemodynamic consequences; however, chest compression quality in this population is often suboptimal. While common, the benefit of step stool use during pediatric CPR has not been studied.
Objective:
We aimed to analyze the effect of step stool use on chest compression quality (depth, rate) in a pediatric emergency department (ED).
Design/Methods:
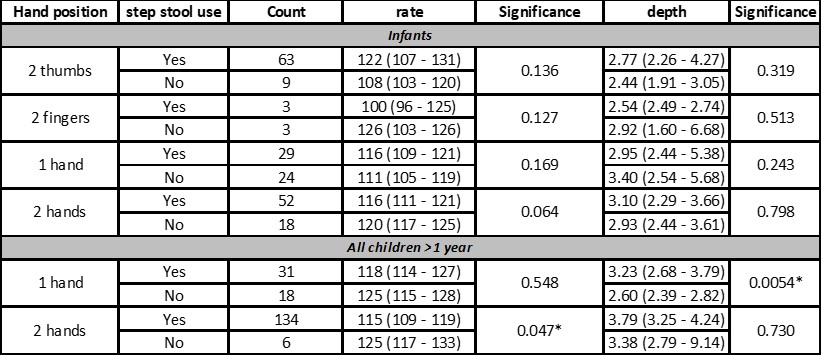
We conducted a prospective observational cohort study involving patients < 8 years of age receiving chest compressions in an ED for >2 minutes. Data was collecting via structured video review and from a CC monitoring device. Analysis was by compressor segment. We compared CC rate and depth by step stool use in each of 3 age groups: < 1 year, 1-8 years, 9-18 years. We also examined step stool and CC quality by compressor hand position: 1) two thumbs, hands encircling chest (2T), 2) two fingers, 2nd and 3rd digits, pressing on anterior sternum (2F), 3) one hand (1H), and 4) two hands (2H).
Results:
46 patients received 390 CC segments (565 total CC minutes). In patients < 1 year and 1-8 years of age, the majority of compressors utilized a step stool (73% < 1 year; 83.3% 1–8 years). For < 1 year of age, there was no difference in mean CC rate or depth with or without step stool use. In children >1 year, a step stool was associated with deeper chest compressions [3.63cm (IQR 3.07 – 4.17) vs 2.74 cm (IQR 2.39 - 3.24) without, p=0.000] and a mean CC rate more consistent with AHA guidelines [115 compressions per minute (IQR 115 – 128) vs 125 (IQR 110 – 121) without, p=0.0037]. Stratified by hand placement technique, 1H compressions with a step stool achieved greater depth in children >1 year (p< 0.01); 2H compressions with a step stool achieved a more compliant CC rate in children >1 year (p< 0.05).
Conclusion(s): CPR depth failed to reliably meet AHA guidelines regardless of stepstool use across all age categories. However, in children between 1 – 8 years of age, step stool use was significantly associated with higher quality chest compressions. Our findings of better CC depth and rate with one and two hand compressions should prompt further investigation and evaluation of CC technique in the pediatric population. .jpg)