Mental Health
Mental Health 2
388 - Acute severe behavioral disturbance requiring parenteral sedation in pediatric mental health presentations to Emergency Medical Services: a retrospective chart review
Publication Number: 388.231
- EB
Elyssia M. Bourke, MBBS MPH BMedSci FACEM (she/her/hers)
PhD Candidate
Murdoch Children's Research Institute
Pascoe Vale, Victoria, Australia
Presenting Author(s)
Background: There has been a significant increase in pediatric mental health presentations to Emergency Medical Services (EMS). The reasons for this include increasing mental health (MH) disorders and inadequate community supports. A proportion of these young people will develop acute severe behavioral disturbance (ASBD). Safe behavioral containment of those with ASBD is essential; and is often achieved using parenteral sedation, which is how we defined the presence of ASBD in our study.
There is little information on the epidemiology of pre-hospital MH presentations. It is unclear which young people are more likely to experience ASBD. The precipitants for and success of the available management options for these pediatric patients are lacking.
Objective:
To describe epidemiological factors relating to MH presentations of young people in the prehospital setting and define those experiencing ASBD by reviewing parenteral sedation use.
Design/Methods:
We performed a retrospective review of ambulance attendances for children (< 18 years) with MH presentations between July 2018 and June 2019 to a state wide EMS system in Australia for a population of 5.8 million persons. Epidemiological data and information pertaining to pediatric patients requiring parenteral sedation for ASBD and any adverse events were extracted from the records and analyzed.
Results:
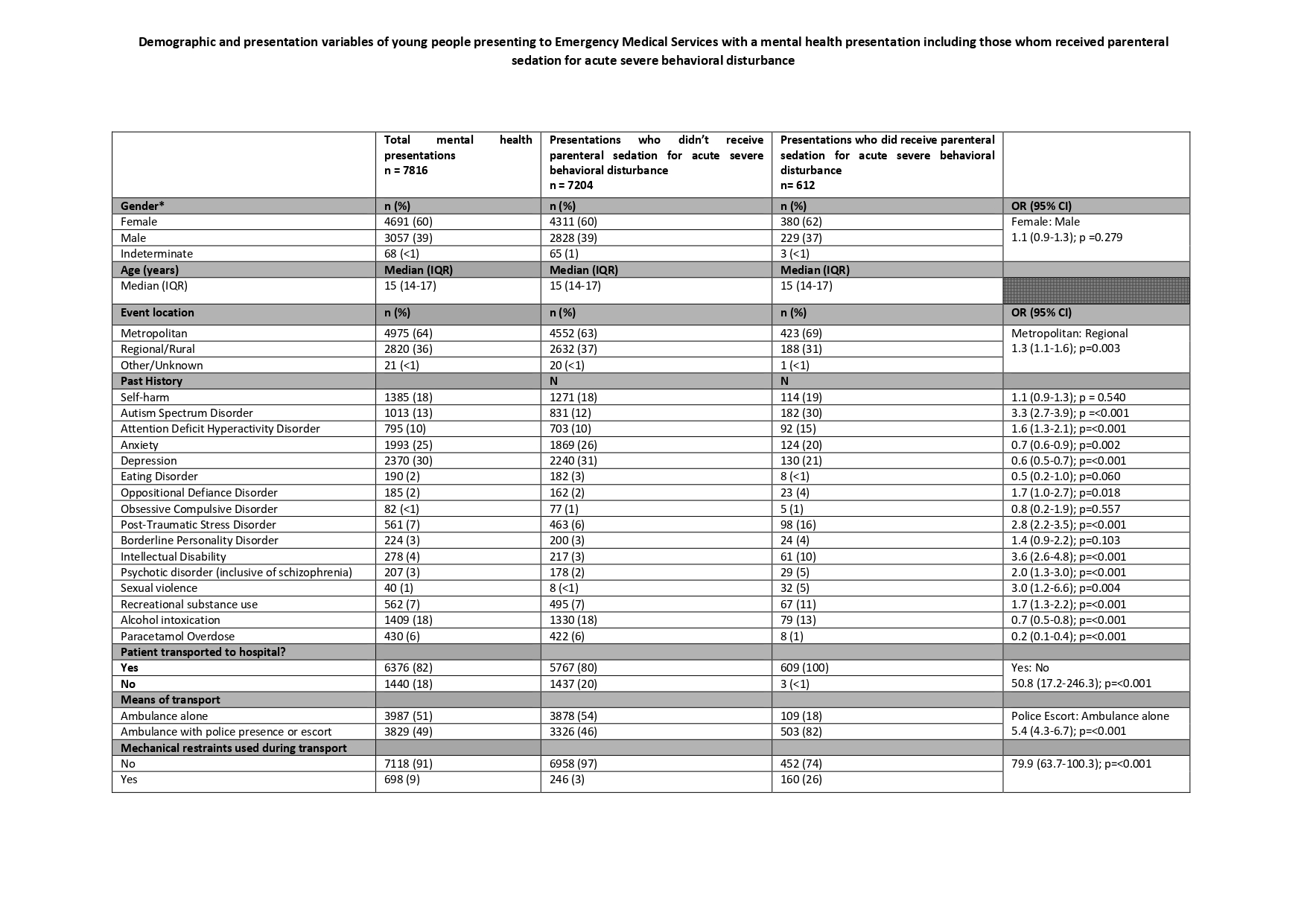
7,816 patients had MH presentations with a median age of 15 years (IQR 14-17) with the majority (60%) being female. These presentations accounted for 14% of all pediatric presentations to EMS.
612 (8%) received parenteral sedation for ASBD.
A number of factors were associated with increased odds of parenteral sedative medication being utilised - autism spectrum disorder (ASD) (OR 3.25, CI 2.68-3.93, p< 0.001), post-traumatic stress disorder (PTSD) (OR 2.8, CI 2.2-3.5, p< 0.001) and an intellectual disability (ID) (OR 3.6, CI 2.6-4.8, p < 0.001).
Police attendance was reported in 82% of cases where sedation was used (OR 5.4, CI 4.4-6.7, p< 0.001) and 26% of this cohort were mechanically restrained (OR 79.9, CI 63.7-100.3, p< 0.001).
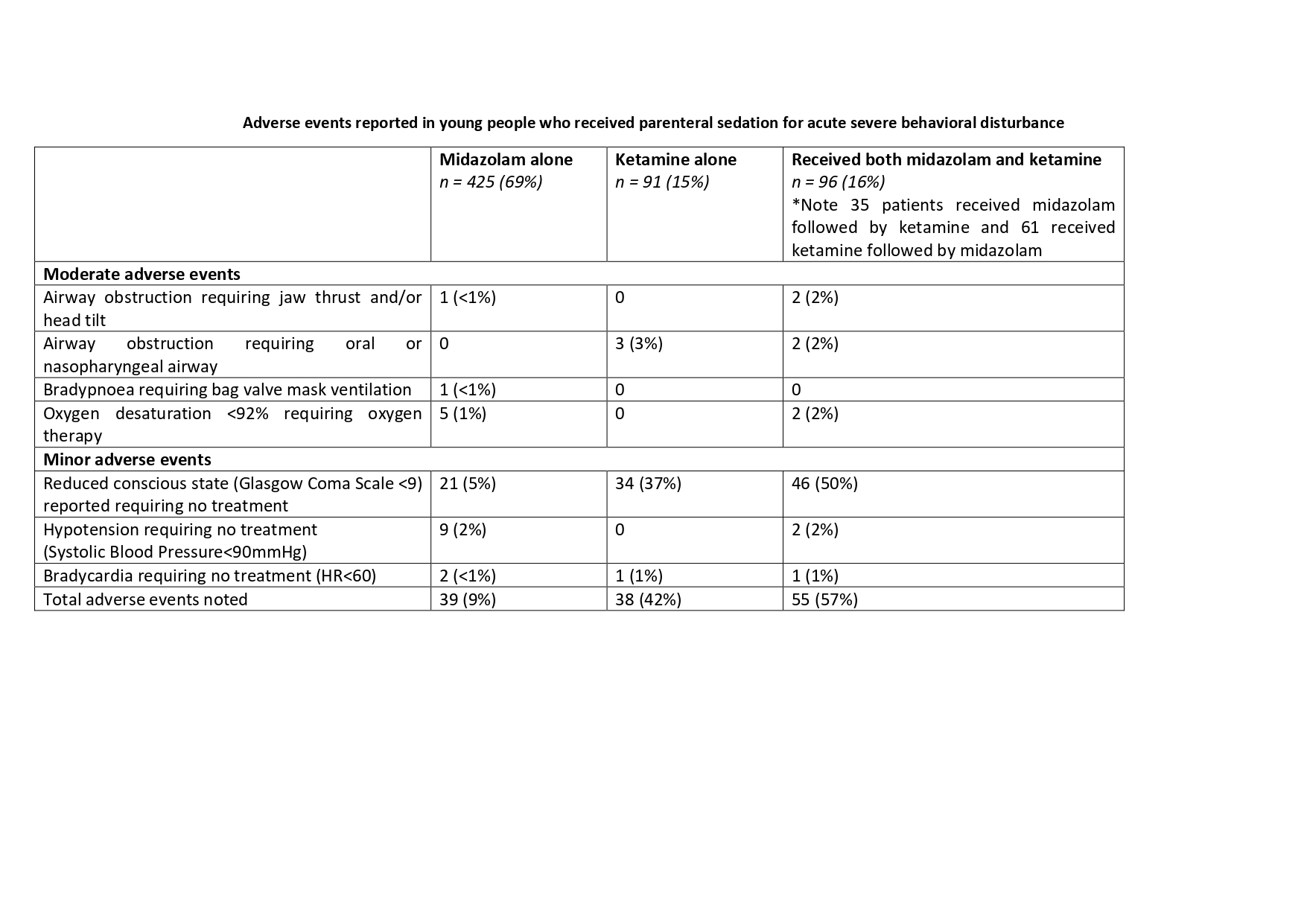
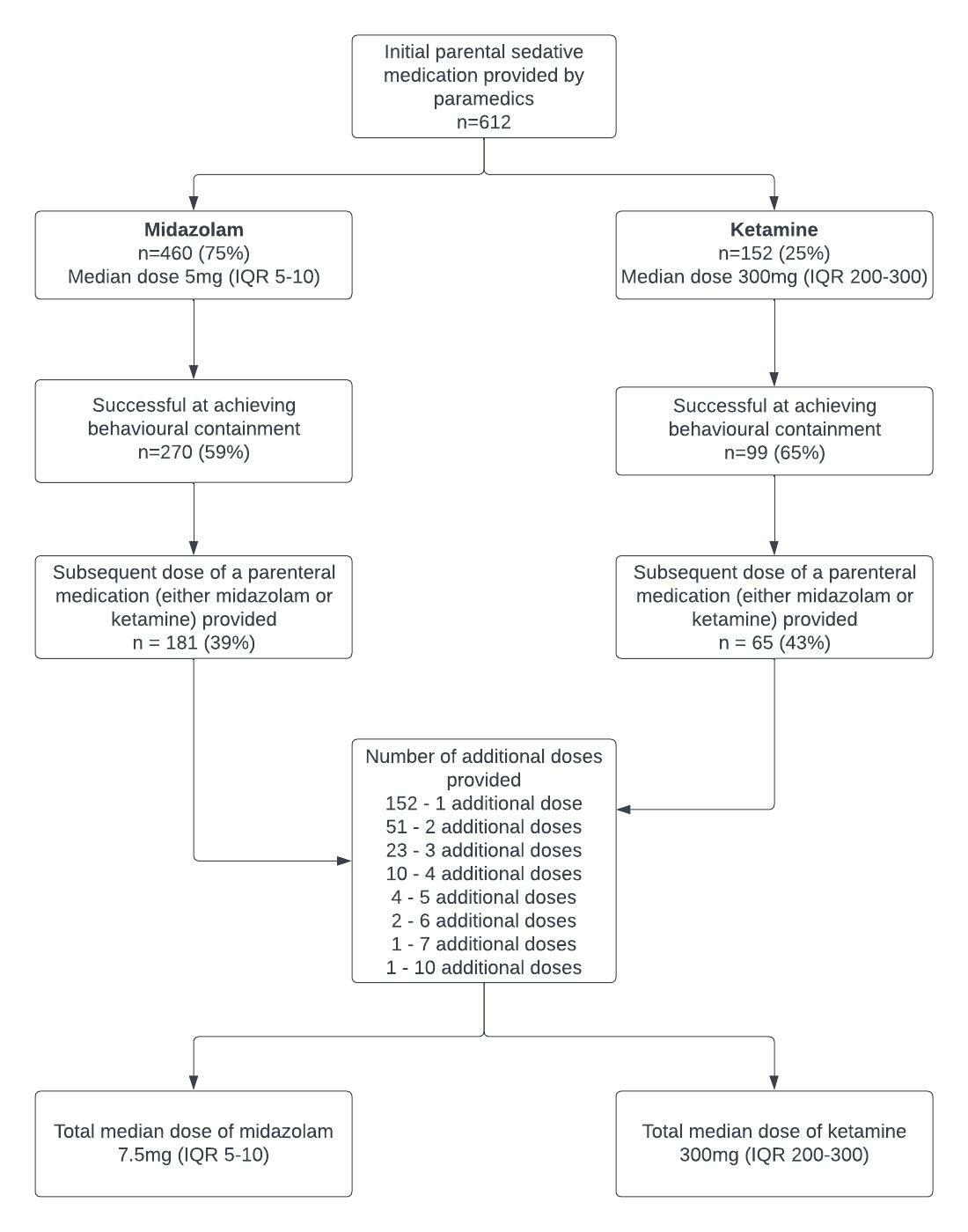
The majority (460, 75%) of young people received midazolam as their first line medication, with the remaining patients provided ketamine (152, 25%). No serious adverse events were noted.
Conclusion(s):
Mental health presentations were a common presentation to EMS. A history of ASD, PTSD or an ID increased the odds of the young person receiving parenteral sedation for ASBD. Sedation appears generally safe in the prehospital setting. Prospective interventional research is required to inform best clinical practice.