Medical Education: Diversity, Equity & Inclusion
Medical Education 8: Diversity, Equity, & Inclusion 2
566 - Simulation-Based Education (SBE) On Racial Themes Through Participation In Maternal-Child Case Scenarios
Publication Number: 566.23

Maya Bunik, MD, MPH (she/her/hers)
Professor. Pediatrics
University of Colorado School of Medicine, Children's Hospital Colorado
Aurora, Colorado, United States
Presenting Author(s)
Background:
Simulation-Based Education (SBE) benefits have been shown within clinical specialties for issues such as giving bad news to a patient or allowing healthcare providers to practice certain procedures. Research continues to indicate that infants born to Black mothers die at twice the rate as their non-Hispanic, White counterparts, regardless of household education level and socioeconomic status. Institutional and structural racism contribute to the social isolation, toxic stress, incidence of pre-term birth and infant mortality rates among US-born Black mothers and their families.
Objective:
The Center for Advancing Professional Excellence (CAPE) at Anschutz Medical Campus of University Colorado, members of the Children’s Colorado Child Health Advocacy Institute, along with engaged community partners and providers, set out to develop maternal-infant case scenarios based on the experience of community members and pilot through SBE increasing awareness of implicit and systemic bias, use of language and identifiers, improving patient-physician relationships as well as provider self-evaluation and reflection regarding the racial and health inequities in patient-family encounters.
Design/Methods:
We used a ‘snowball approach’ to recruit providers and community partners that had been meeting from 2018-2019 through Black Health Initiative development sessions at Children’s Hospital Colorado. From 2020 to present, these trainings were extended beyond the internal team (n=30 providers; n=30 community advocates). During the half-day workshop, participants participated in a brief didactic presentation introducing goals and then proceeded through the SBE. Fidelity of the 3 intervention scenarios was maintained with scripts by trained specialized patients (e.g. mother and teenage daughter whose premature infant had died; isolated mother who was struggling with breastfeeding and a disappointed mother who was rescheduled because she was late to a telehealth visit).
Results:
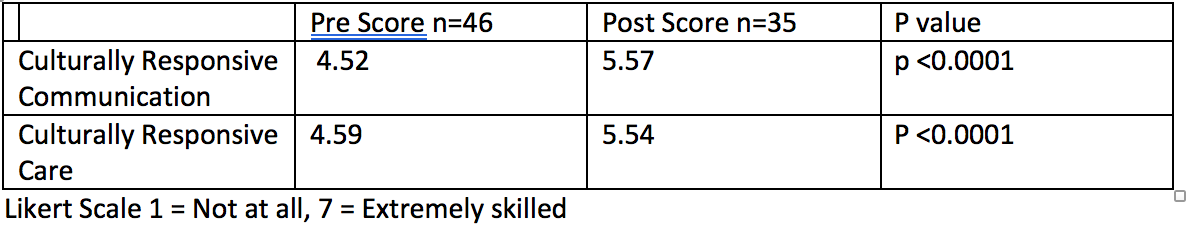
Feedback was provided by the patient-actors and an observation team. Pre and post training scores are shown in Table 1. Participants debriefed for 30 min after the 3 scenarios were completed. Take-away themes included: a. Commit to continued growth/skills acquisition; b. Ask more open-ended questions; c. Demonstrate empathy, perspective taking.
Conclusion(s):
Participants reported high satisfaction with this activity. Dissemination and larger scale evaluation may prove that this is an effective way for clinical providers to make changes with regards to their approach to addressing racism in visits with marginalized families.