Emergency Medicine: Quality Improvement
Emergency Medicine 5 B
347 - Use of a Novel Workload-to-Room Ratio to Examine Operational Outcomes in a Pediatric ED
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 347
Publication Number: 347.209
Publication Number: 347.209
Kaleena Patel, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Xianqun Luan, The Children's Hospital of Philadelphia, Philadelphia, PA, United States; Rachel Rempell, Children's hospital of philadelphia, Philadelphia, PA, United States; Mercedes M.. Blackstone, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Joseph J. Zorc, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Brandon Ku, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Daniel Corwin, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Kaleena Patel, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Pediatric emergency departments (PEDs) often struggle with optimal staffing (adequate staff for patient volume and acuity). Traditionally, staffing models are static or based on seasonal volume trends. A novel algorithm was developed to identify “workload,” incorporating volume and effort required to care for ED patients. However, the association between this model and operational outcomes is unknown.
Objective: Determine correlation between workload to room ratio (WRR) and operational outcomes.
Design/Methods: We evaluated data over 1 year from July 2018-June 2019 (FY19) at an urban, academic, tertiary care children’s hospital. We used hospital financial charges from coded review as a surrogate for the “workload” necessitated for each patient, transformed into a weighted hourly workload by dividing charges by mean length of stay for each billing category. We created total ED workload per hour by summing individual hourly workload values and created the WRR by incorporating the number of staffed rooms (WRR range 0-9). We then identified the ideal WRR range from 2018 (< 3.3; excluding the upper quartile). We calculated the mean daily WRR and % hours/day in the ideal range for FY19. We utilized a Pearson correlation coefficient (r) with 95% confidence intervals (CI) to assess the correlation between mean daily WRR, %hours/day in ideal WRR range, mean daily patient volume, and four operational outcomes: (1) % triage level 4-5 patients discharged in 2 hours; (2) % asthma patients receiving steroids within 1 hour; (3) % sepsis patients receiving antibiotics within 1 hour; (4) % oncologic patients with fever receiving antibiotics within 1 hour.
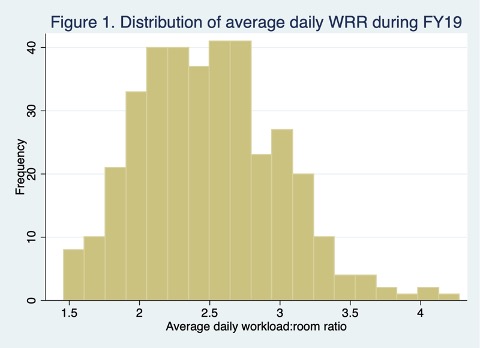
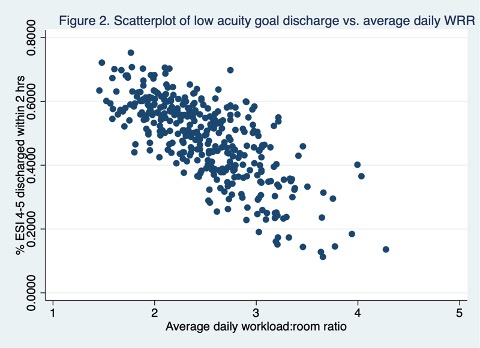
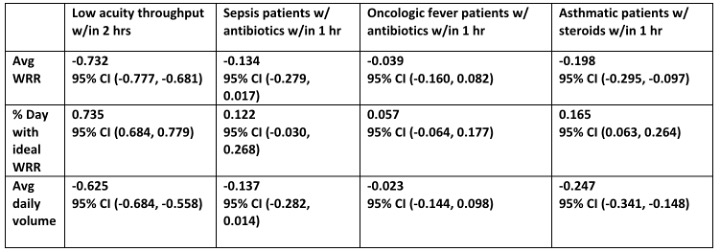
Results: Mean WRR for FY19 was 2.50 (CI 2.45 to 2.55) (Fig 1). There was a strong correlation between % low acuity discharges within 2 hours and mean WRR (r= -0.73, CI -0.78 to -0.68) (Fig 2), and % hours in ideal WRR (r= 0.735, CI 0.68 to 0.78), significantly stronger than with mean daily volume (r= -0.63, CI -0.68 to -0.56). For disease-specific operation outcomes there was at most a weak correlation with mean WRR, % hours in ideal WRR, and volume (Table 1).
Conclusion(s): WRR is more strongly associated with throughput of low acuity PED patients compared to patient volume. Neither WRR nor volume was significantly associated with disease-specific operational outcomes. Additional comparisons (patient satisfaction, educational metrics, other disease-specific outcomes) may be made to assess the validity of WRR compared to patient volume; however, with current operational outcome data, it is evident this novel WRR has the potential to inform future dynamic staffing models.