Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 2
664 - Antimicrobial usage in tertiary neonatal intensive care units in Canada: a 10-year review
Publication Number: 664.241
Joseph Ting, MBBS, MPH
Associate Professor
University of Alberta
Edmonton, Alberta, Canada
Presenting Author(s)
Background:
Antimicrobials are the most common medication prescribed in the neonatal intensive care unit (NICU). Excessive antimicrobial exposure is associated with an increase in neonatal mortality, morbidities, and adverse neurodevelopmental outcomes. Canadian Neonatal Network (CNN) has been promoting judicious antimicrobial use through Evidence-based Practice for Improving Quality processes throughout the years.
Objective:
To evaluate the trend of antimicrobial consumption and clinical sepsis episodes in tertiary NICU in Canada in the past decade
Design/Methods:
This is a retrospective cohort study including data from infants born at < 33 weeks gestational age (GA) admitted to 32 NICUs in the CNN between Jan 1, 2012, and Dec 31, 2021. Antimicrobial utilization rate (AUR) is defined as the number of days with ≥1 antimicrobial divided by the total patient days. Clinical sepsis referred to infants receiving antimicrobials for ≥5 consecutive days in the absence of positive blood or cerebrospinal fluid cultures. Reporting of benchmarked AUR across CNN started in 2016, and a nationwide Antimicrobial Stewardship Program started in 2019. The trends of sepsis and antimicrobial use were evaluated according to early (2012-2015), mid (2016-2018), and recent (2019-2021) phases. Subgroup analyses were performed among infants without culture-proven sepsis or necrotizing enterocolitis (NEC)≥Stage 2 and those born at < 29 weeks GA.
Results:
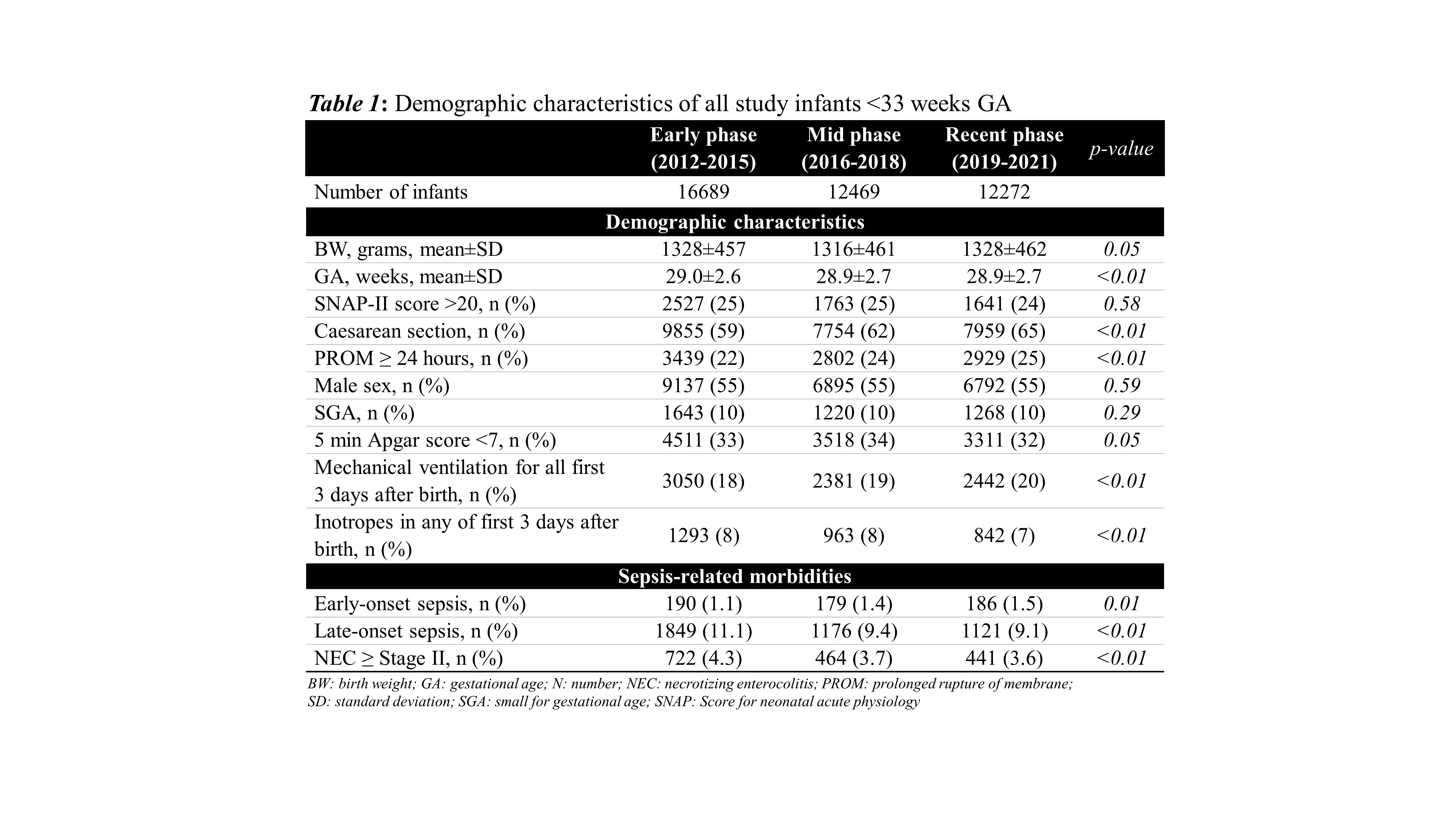
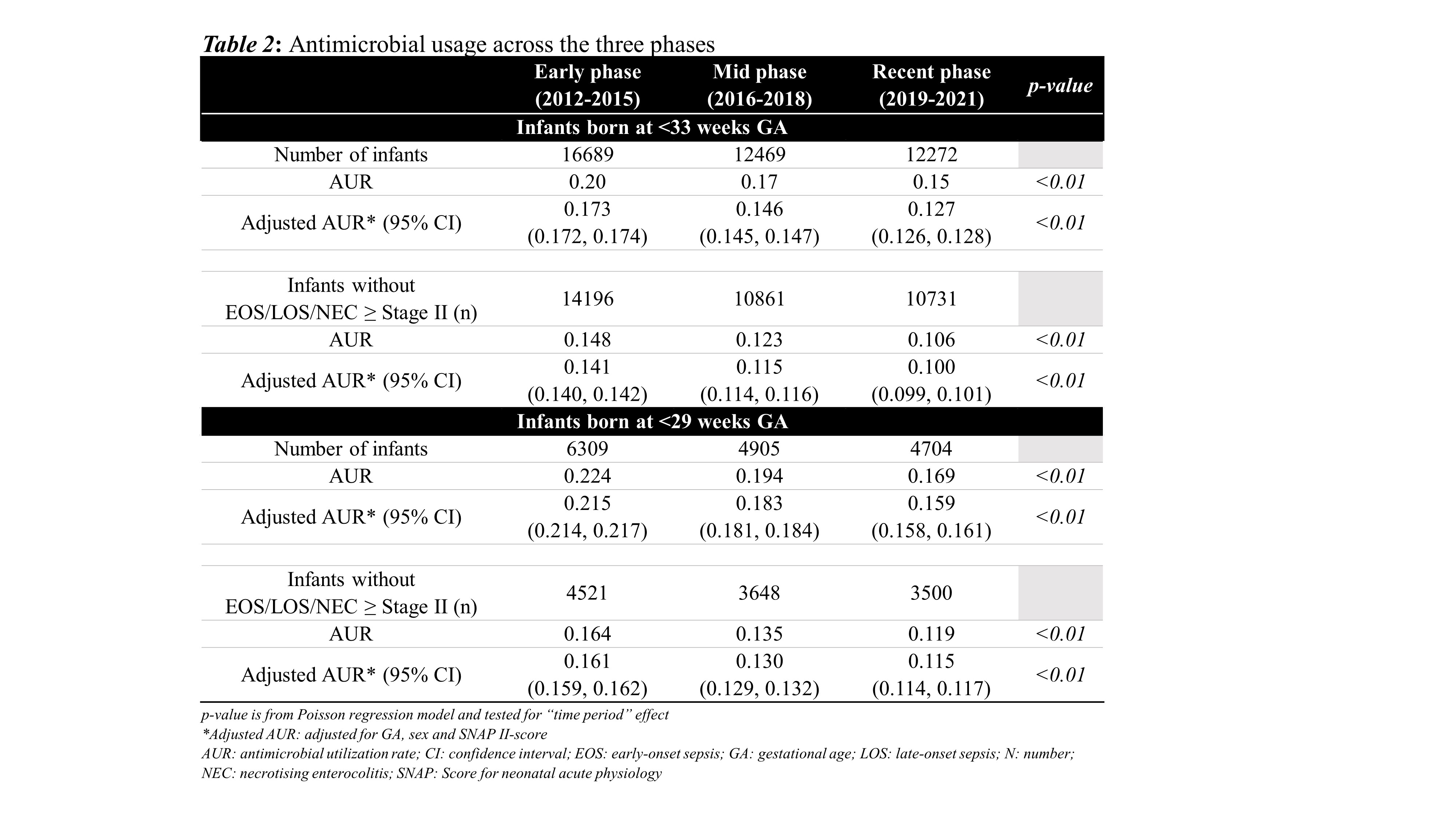
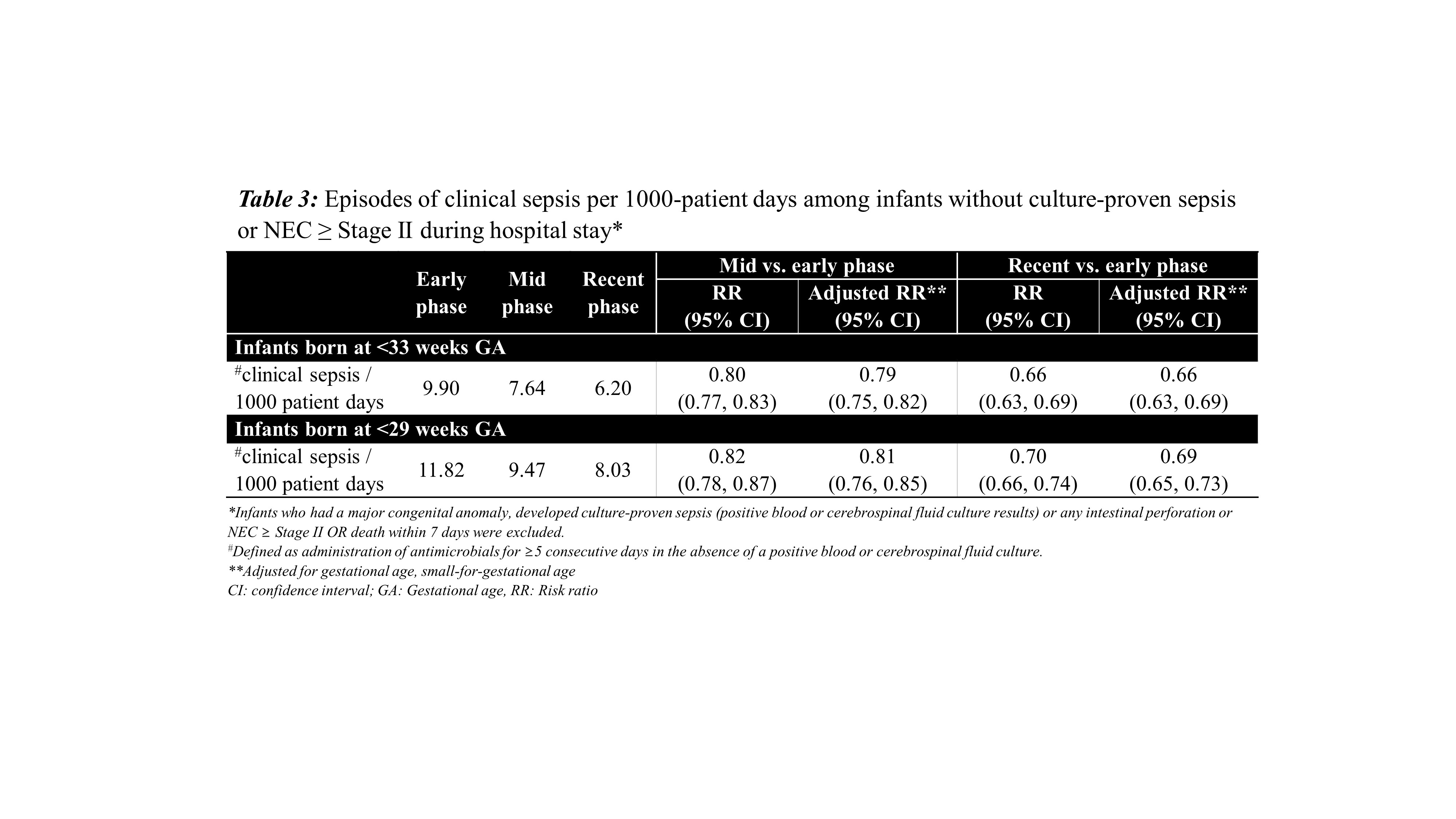
After excluding 1768 infants who had a major congenital anomaly or were moribund on admission, 41430 infants were included in this work. An increasing trend of early-onset sepsis (1.1% to 1.5%, p=0.01), and a decreasing trend of late-onset sepsis (11.1% to 9.1%, p< 0.01), and NEC (4.3% to 3.6%, p< 0.01) were found across the time periods [Table 1]. AUR showed a decreasing trend from 0.148 to 0.106 (p< 0.01) among infants without any culture-proven sepsis or NEC Stage≥2 [Table 2]. Proportion of infants without culture-proven sepsis or spontaneous intestinal perforation/NEC but receiving antimicrobials >3 days within the first week decreased from 34% to 19% over the study period (p< 0.01). The number of clinical sepsis episodes decreased from 9.9 to 6.2/1000 patient-day (adjusted OR=0.66, 95%CI [0.63, 0.69]) [Table 3]. The decreasing trends of aforementioned analyses were also observed in the subgroup analyses of infants born at < 29 weeks GA.
Conclusion(s):
There was a significant decline in AUR and clinical sepsis episodes among infants born at < 33 weeks GA over the past decade in tertiary NICU in Canada.