Hospital Medicine: Education
Hospital Medicine 3
495 - The Community Pediatric Hospital Medicine Individualized Curriculum: Recommended Experiences
Publication Number: 495.221
Shivani Patel, DO, MEd, MS (she/her/hers)
Assistant Professor of Pediatrics
Cincinnati Children's Hospital Medical Center
Mason, Ohio, United States
Presenting Author(s)
Background: As pediatric hospital medicine (PHM) continues to grow and now has subspecialty accreditation, increasing number of residents are choosing this career path. Through the implementation of PHM fellowships and core competencies of PHM, trainees are encouraged to seek experience in the care of complex medical patients and surgical co-management, as well as in non-clinical areas. Pediatric residents may choose not to pursue fellowships or may not match into fellowship due to increasing interest and limited available positions and may seek opportunities in community PHM (CPHM). While university-based PHM recommendations have been described; resources for pediatric residents interested in pursuing a career in CPHM are lacking. It is imperative to identify experiences to benefit residents entering this field.
Objective: The goal of our study was to identify experiences and activities that would enhance career preparation for residents interested in CPHM.
Design/Methods:
This was a cross sectional national electronic survey of community pediatric hospitalists to identify experiences, electives, and procedures to better prepare residents for a career in the CPHM setting. Descriptive statistics were used to analyze data.
Results:
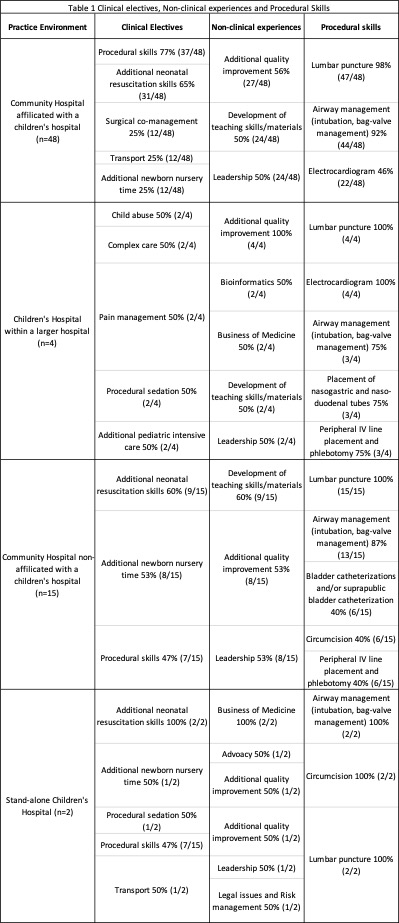
The survey had a response rate of 21% (69/331). 70% (48/69) were hospitalists who spent most of their clinical time in a community hospital affiliated with a university. 88% (61/69) of all respondents noted their residency did not have a pathway for residents who were interested in pursuing PHM. 48% (33/69) respondents rotated through a community PHM setting during residency; 66% (21/32) perceived this influenced their decision to practice in a community setting. Recommended clinical electives were procedural skills (65%, 45/69), additional neonatal resuscitation/delivery skills (62%, 43/69) and additional newborn nursery time (30%; 21/69). Recommended nonclinical electives were additional quality improvement training (58%, 40/69), leadership (51%, 35/69) and development of teaching skills and materials (51%, 35/69). Procedural skills recommended were lumbar puncture (99%, 68/69), airway management (90%, 62/69) and electrocardiogram interpretation (46%, 32/69). All respondents felt these recommendations should be supplemented with mentorship. Table 1 includes the breakdown of clinical, nonclinical electives and procedural skills recommended by the hospitalist subgroup.
Conclusion(s): Identification of key clinical experiences and non-clinical activities for residents interested in pursuing CPHM may assist with improved career preparedness of residents entering this field.