Hospital Medicine: Education
Hospital Medicine 3
494 - Psychological safety during family-centered rounds: how do residents’ sense of safety align with families’ perspectives on learning?
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 494
Publication Number: 494.221
Publication Number: 494.221
Shweta Bhatia, University of Colorado School of Medicine, Denver, CO, United States; Ge Yan, Children's Hospital Colorado, Denver, CO, United States; Leonard Seltz, University of Colorado School of Medicine, Denver, CO, United States
.jpg)
Shweta Bhatia, MD (she/her/hers)
Resident
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Family-centered rounds, multi-disciplinary bedside rounds conducted in the presence of families, may not provide an optimally safe learning environment. Important for resident education, psychological safety is the perception that it is safe to take interpersonal risks. Yet, literature exploring resident psychological safety during rounds is scarce, and it remains unclear if safety concerns are founded on families’ views.
Objective: Our study aimed to 1) describe residents’ perspectives on the psychological safety of family-centered rounds, and 2) explore families’ views on rounds as a place for learning.
Design/Methods: Using a qualitative phenomenological approach, we conducted three focus groups with 14 residents (10 PGY-1s, four PGY-3s) and interviews with 10 parents of children on hospital medicine services from October to November 2022. Three investigators analyzed the data with the constant comparative method. Codes were developed with an iterative approach and organized into themes. Discrepancies were resolved by consensus.
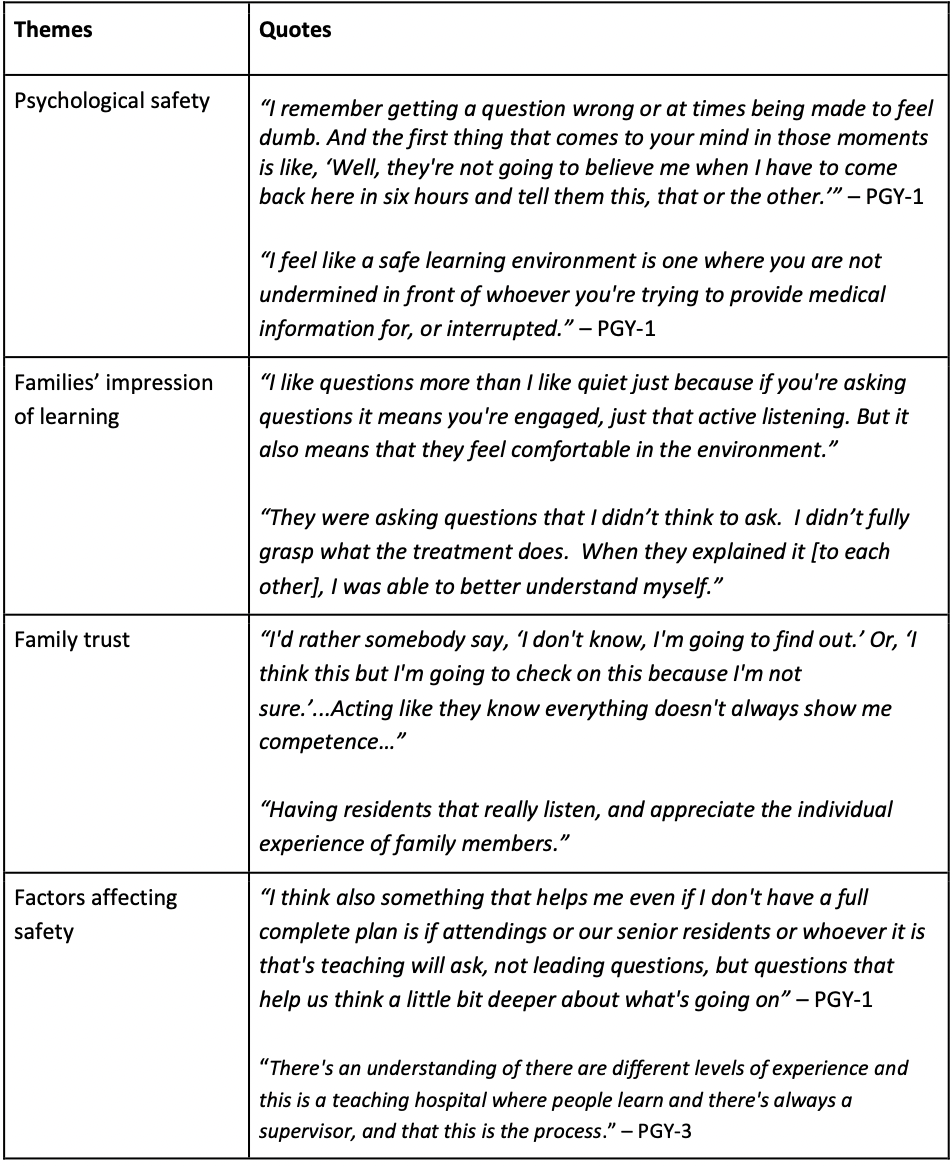
Results: Four themes were identified: psychological safety, families’ impression of learning, family trust, and factors affecting safety (Table 1). Residents described psychological safety as feeling comfortable with asking and answering questions, proposing a plan of care, being wrong, and not getting judged. Some residents felt psychologically safe during rounds; others did not, raising concerns about losing trust of families or appearing incompetent. Yet, many families acknowledged rounds as important for experiential learning and collaboration and expected learners to ask questions. Some parents described how questions among team members promoted their own understanding of the care plan. Learning during rounds did not typically influence level of family trust in residents. Instead, families viewed residents who listened, were empathetic, and understood the patients’ condition as competent and trustworthy. Parents acknowledged the different levels of experience among the health care team, and some felt more comfortable having attending oversight. Factors that increased resident psychological safety included team dynamics, such as camaraderie and respect, a positive supervisor response to resident input, and setting expectations for education.
Conclusion(s): Residents’ level of psychological safety varied. Factors that residents perceived as resulting in loss of family trust largely differed from families’ perspectives. Setting team member and family expectations for learning during rounds may help optimize psychological safety.