Hospital Medicine: Systems/Population-based Research
Hospital Medicine 4
500 - Changes in Texas Asthma Hospitalizations During the COVID Pandemic by Socioeconomic Status
Publication Number: 500.221
Raymond Parlar-Chun, MD
Associate Professor of Pediatrics
McGovern Medical School at the University of Texas Health Science Center at Houston
Houston, Texas, United States
Presenting Author(s)
Background:
Hospitals experienced a decreased incidence of asthma admissions during the height of the COVID pandemic. It is unknown whether this decrease was consistent for all patients of all socioeconomic status (SES).
Objective:
To determine changes in hospitalization rates during the pandemic stratified by SES. We hypothesize patients from low SES zip codes had less change given potentially exacerbated social barriers to care brought about by the pandemic.
Design/Methods:
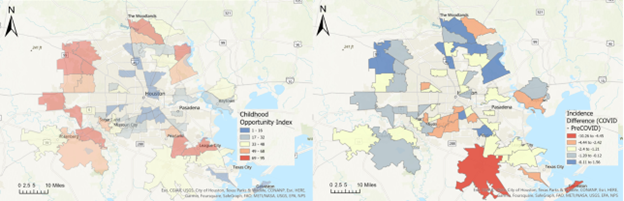
Hospitalization data was obtained from 2019-Q1 to 2021-Q4 from the Texas Inpatient Public Use Data File. ICD 10 code of J45xx as the admitting, principal, or first other diagnosis code was classified as an asthma admission. Hospitalization incidence rates were calculated as admissions/10,000 children by quarter. Patient zip code was matched with the Childhood Opportunity Index (COI) to determine SES. Zip codes with more than 30 observations were included. Nationally normed continuous COI data and state normed categorical classifications were used to classify SES. Analysis included descriptive statistics, ANOVA testing, Pearson’s correlation, and linear regression. Geospatial mapping with ArcGIS was performed on large metropolitan areas for visualization of any region-based patterns.
Results:
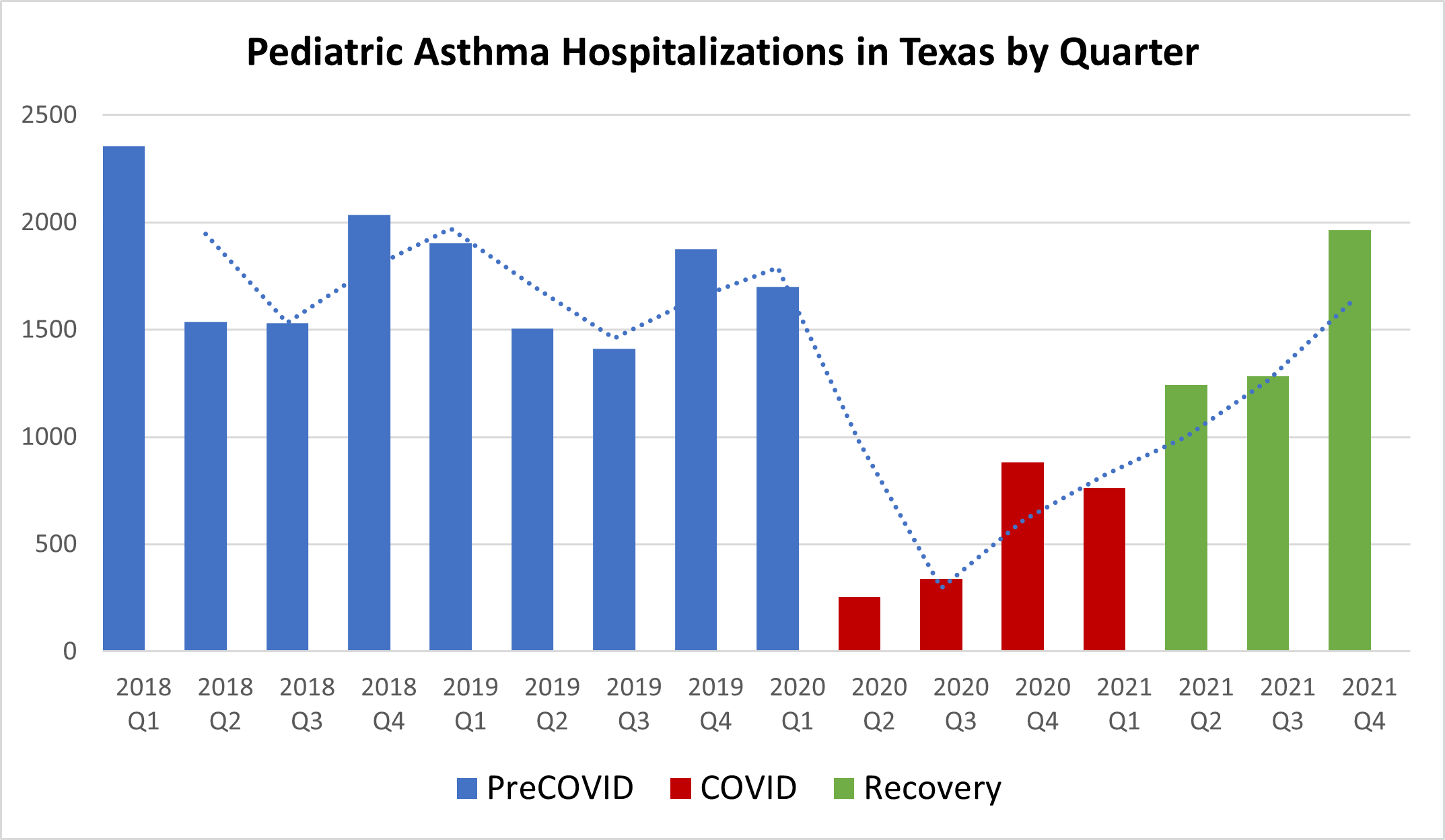
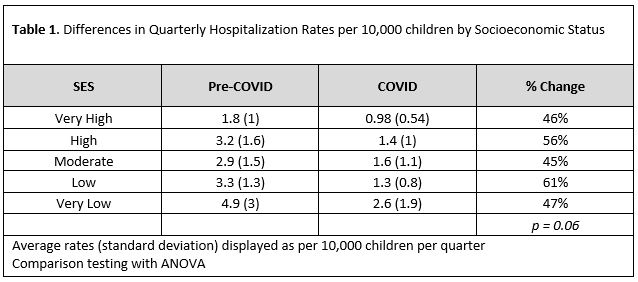
A total of 22,584 pediatric hospitalizations were obtained with 1298 unique zip codes. 144 zip codes had more than 30 observations. 22 (15%) zip codes were from very high, 22 (15%) from high, 25 (17%) from moderate, 31 (22%) from low, and 44 (31%) from very low COI. The average incidence of asthma hospitalizations/quarter/10,000 children in the pre-COVID period was 3.48 (2.25), 1.72 (1.4) during COVID, and 3.35 (2.13) in the recovery period. FIGURE 1. When stratified by SES, changes ranged from 45% - 61% decreases with no significant differences between groups. TABLE 1. Correlation between COI and percent change was 0.08, and regression also did not show a significant relationship. While geospatial mapping showed larger absolute changes in zip codes of lower SES (FIGURE 2) patterns in relative changes were inconsistent.
Conclusion(s):
The incidence of asthma hospitalizations dropped by ~50% during the height of the COVID pandemic. This drop was consistent among SES categories. Despite similar relative drops, patients from the lowest SES continued to have more than 2.5 times the rate of hospitalization compared to patients from the highest SES. While interventions during the pandemic show that hospitalization rates can be cut in half, there remain potentially unmodifiable barriers that place patients of low SES at higher risk for asthma hospitalization.