Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 5
447 - Navigating COVID-19 Vaccine Hesitancy Among Black, Indigenous and People of Color (BIPOC) Communities in 2021
Publication Number: 447.219

Jade Sanders, MD, MPH, FAAP (she/her/hers)
Instructor of Pediatrics
Children’s National Hospital/The George Washington University School of Medicine and Health Sciences
Washington, District of Columbia, United States
Presenting Author(s)
Background:
According to the Centers for Disease Control and Prevention, racial disparities in the percentage of people with at least one dose of the COVID-19 vaccine exist among those fully vaccinated. Similarly, the Kaiser Family Foundation found disproportionately low COVID-19 vaccine uptake in BIPOC communities with increased burdens of COVID-19 deaths nationally.
Objective:
This qualitative study aims to improve understanding of how underrepresented minority (URM) healthcare professionals, who witness and experience contradicting historical, racial, and scientific arguments, navigate the complex climate of COVID-19 in America and use their influence and expertise to combat low COVID-19 vaccine uptake among BIPOC communities. Data obtained will be used to develop recommendations for improving COVID-19 vaccine administration in BIPOC communities.
Design/Methods:
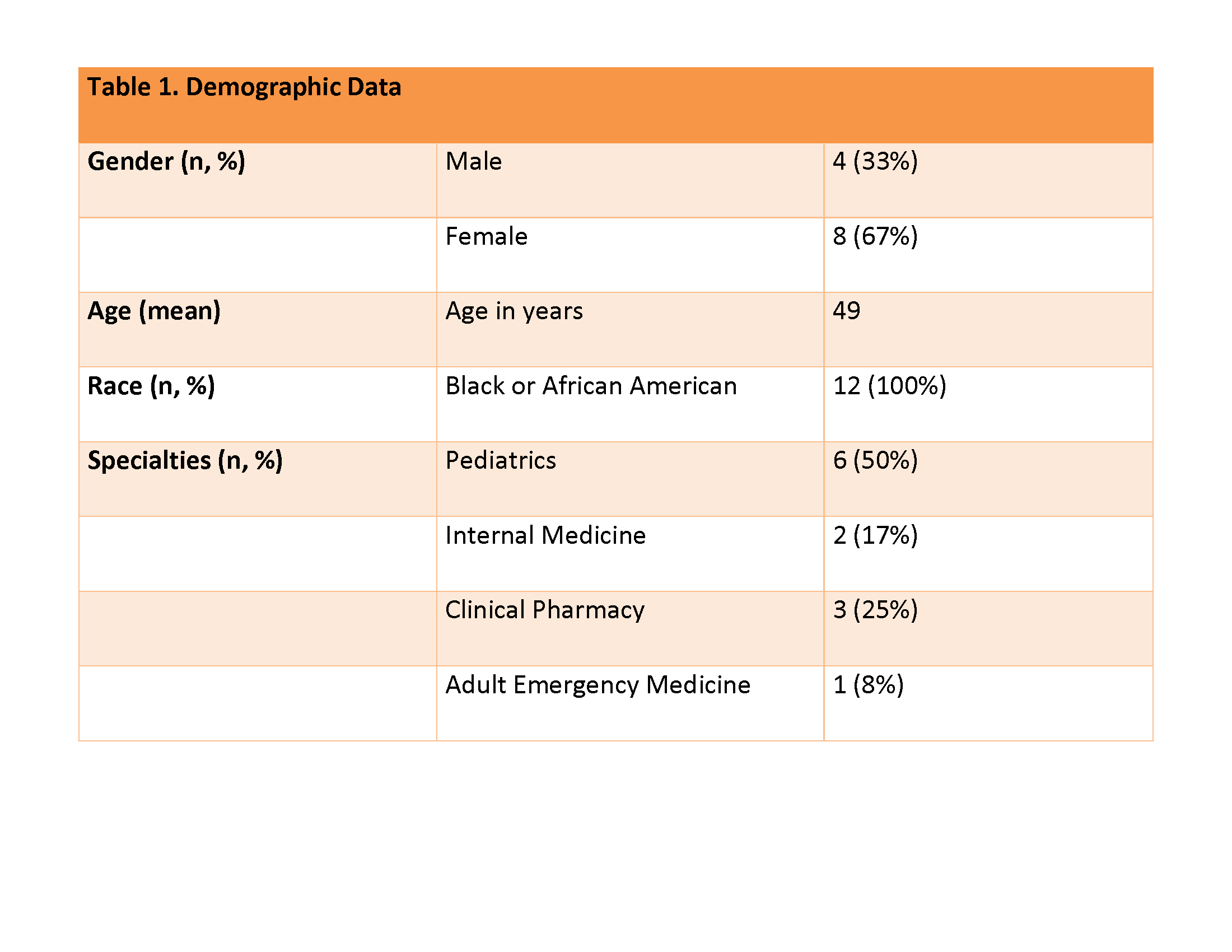
Using a phenomenological framework (Figure 1), the study invited 15 URM professionals in various roles in the healthcare system, with nearly 250 years of experience collectively (Table 1), to discuss observations of low COVID-19 vaccine receptivity in their community, personal reflections on the vaccine roll-out, and their personal view on self-vaccination. The cohort constituted authors from an anthology exploring how URM healthcare workers confront racism, health disparities, and the trauma of COVID-19. Excluded participants were non-clinical or opted out. Inductive study methods were used to elucidate novel and shared perspectives among interviewees.
Results:
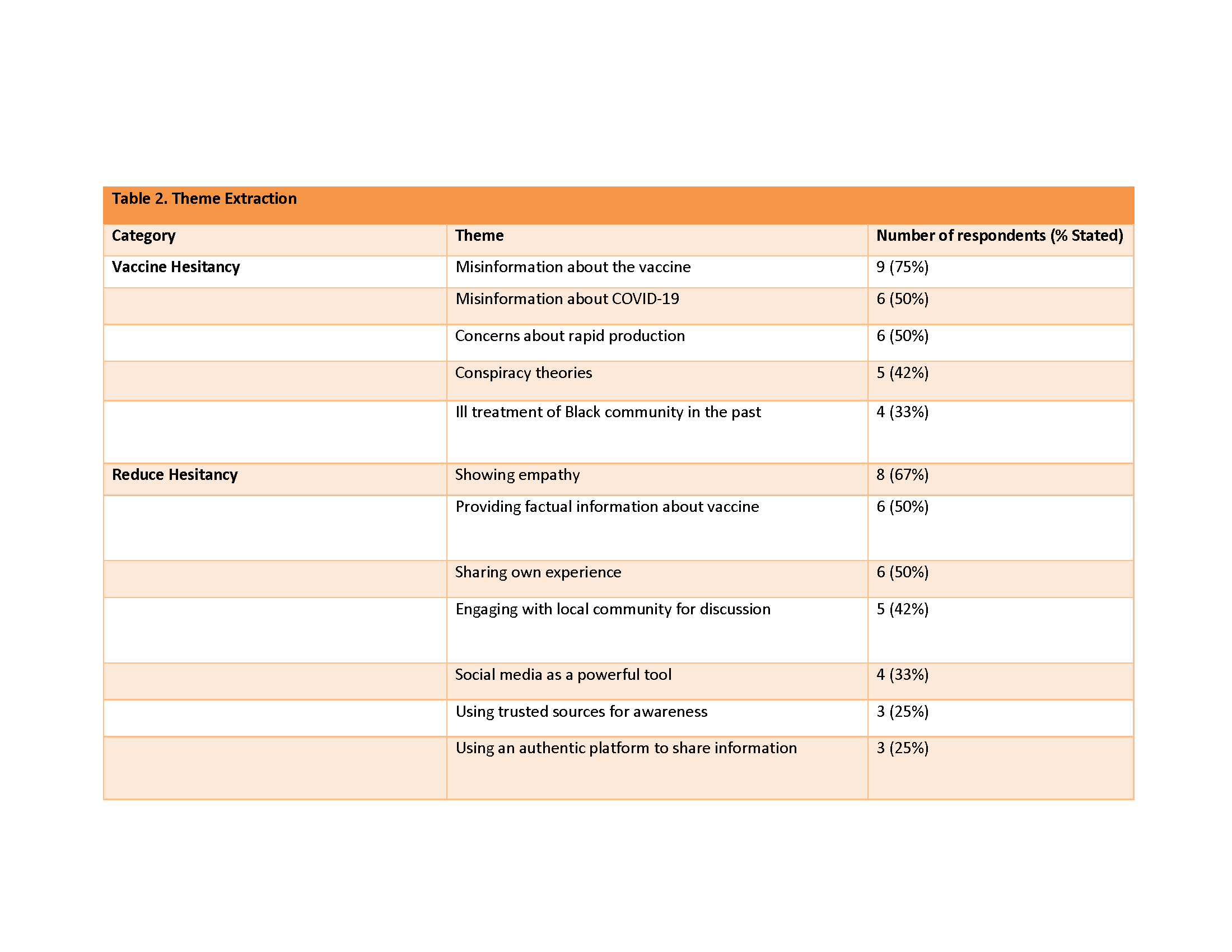
Observations about vaccine hesitancy involved the following common themes (Table 2): concerns about misinformation about the vaccine (75%, 9/12); misinformation about COVID-19 and concerns about rapid production (50%, 6/12); conspiracy theories (42%, 5/12), and ill treatment of the Black community in the past (33%, 4/12). The following common strategies were used or recommended to reduce hesitancy: showing empathy (67%, 8/12); providing facts about the vaccine and sharing their own experiences (50%); engaging with local community for discussion (42%), social media (33%, 4/12); using trusted sources for awareness and using an authentic platform to share information (25%, 3/12).
Conclusion(s):
Future investigations with larger cohorts are encouraged to evaluate the effectiveness of these strategies as interventions. We recently conducted an additional 22 interviews to expand this research and suggest that others do the same to help us address the topic of vaccine hesitancy among BIPOC communities, real or perceived..png)