Children with Chronic Conditions
Children with Chronic Conditions 2
291 - Care Beyond the Bedside: The More You Do, the More You CAN-DO
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 291
Publication Number: 291.204
Publication Number: 291.204
Claire Wallace, Ranken Jordan Pediatric Bridge Hospital, Saint Louis, MO, United States; Patrick Hogan, Ranken Jordan Pediatric Bridge Hospital, Saint Louis, MO, United States; Nicholas Holekamp, Ranken Jordan Pediatric Bridge Hospital, St. Louis, MO, United States; Duha Al-Zubeidi, Ranken Jordan Bridge hospital, maryland heights, MO, United States; Nanette Schaffer-Nay, Ranken Jordan Pediatric Bridge Hospital, Maryland Heights, MO, United States

Claire Wallace, PhD (she/her/hers)
Pediatric Psychologist
Ranken Jordan Pediatric Bridge Hospital
Saint Louis, Missouri, United States
Presenting Author(s)
Background: Chronically hospitalized children are at risk for neurodevelopmental delay, compounded by restricted social interactions, movement, and environmental stimulation. Increased focus on how and where hospitalized children spend their time will help inform hospital programming to mitigate the effects of hospitalization.
Objective: We measured the movements and interaction of inpatients with medical complexity in a pediatric post-acute care specialty hospital to (1) characterize developmentally relevant aspects of our inpatient environment and (2) inform developmental programming to mitigate deficiencies created by long term hospitalization.
Design/Methods: As a quality improvement initiative to inform neurodevelopmental programming for children with medical complexity at our pediatric post-acute care specialty hospital, we conducted >232 hours of time-motion observations. Trained observers followed 0-5-year-old inpatients from 7am-7pm on weekdays, categorizing observations within five domains: Where, With, Position, State, Environment. Observations were collected continuously utilizing REDCap on iPads. A change in any domain initiated a new observation.
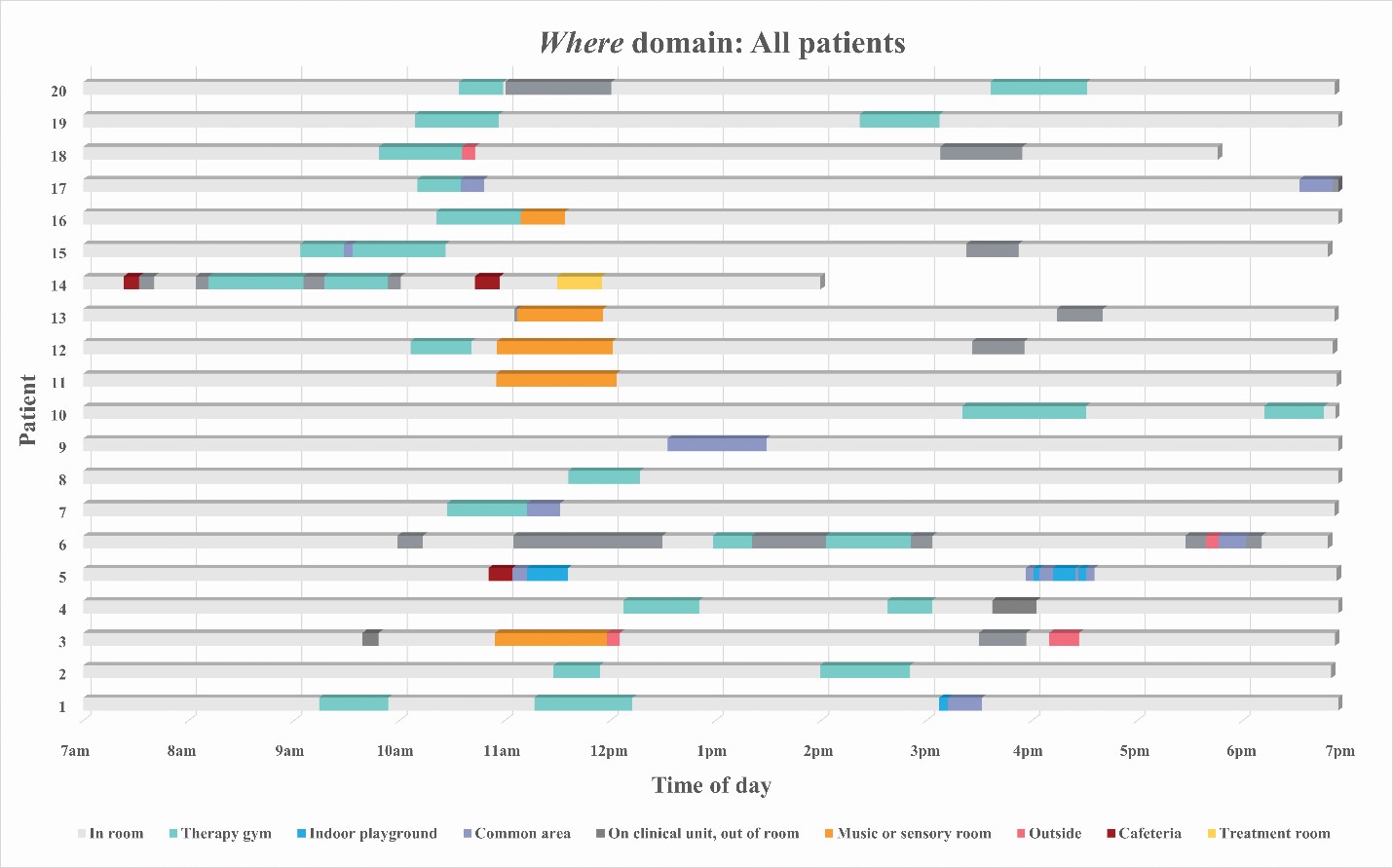
Results: Patients were median 1 year and 8 months of age (range 2 months - 3 years 9 months) with a median length of hospitalization of 514 days (range 66 - 1298). In total, 2636 unique observations (or median 134 observations per patient-day [range 95 – 210]) were collected. Patients left their rooms up to 4 times per day for median 1 hour (h) and 34 minutes (m) (range 41m - 4h:30m); see Figure. Patients spent 4h:6m (2h:57m - 6h:30m) interacting with someone and 3h:51m (57m - 6h:36m) out of bed each day. Patients were simultaneously out of their beds, interacting with someone, and awake for 2h:21m (51m - 4h:19m) each day.
Conclusion(s): Time-motion observations identified 5 focus areas for enriching neurodevelopment: 1) face-to-face interactions; 2) time out of the hospital room; 3) positional variety; 4) sleep-wake schedules; and 5) environmental variety of toys, books, music, and positive touch. Despite a care model prioritizing time out of bed and social interaction, time-motion observations indicate patients spent many of their waking hours in bed and alone. Quantifying our inpatients developmental opportunities informed neurodevelopmental programming initiatives, particularly creation of an Optimization Zone where hospitalized children aged 0-5 can spend time beyond the bedside.