Emergency Medicine: All Areas
Emergency Medicine 6
360 - The Utility of Urine Drug Screens in Patients Presenting to the Emergency Department for a Primary Mental Health Concern
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 360
Publication Number: 360.21
Publication Number: 360.21
Michael B. Bagg, Children's Hospital Colorado, Denver, CO, United States; Jan Leonard, University of Colorado School of Medicine, Aurora, CO, United States; Lilliam Ambroggio, Children's Hospital Colorado, Aurora, CO, United States; Rachel Cafferty, University of Colorado School of Medicine, Aurora, CO, United States

Michael B. Bagg, MD (he/him/his)
Resident Physician
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: The pediatric Emergency Department (ED) is increasingly positioned to screen youth for substance use or abuse and evaluate patients with mental or behavioral health concerns. A urine drug screen (UDS) is often required of youth presenting to the ED for mental health care and subsequently requiring inpatient psychiatric hospitalization. The utility of UDS when youth self-report substance use in the ED is unknown.
Objective: Determine the association between self-report and UDS results at a return mental health encounter.
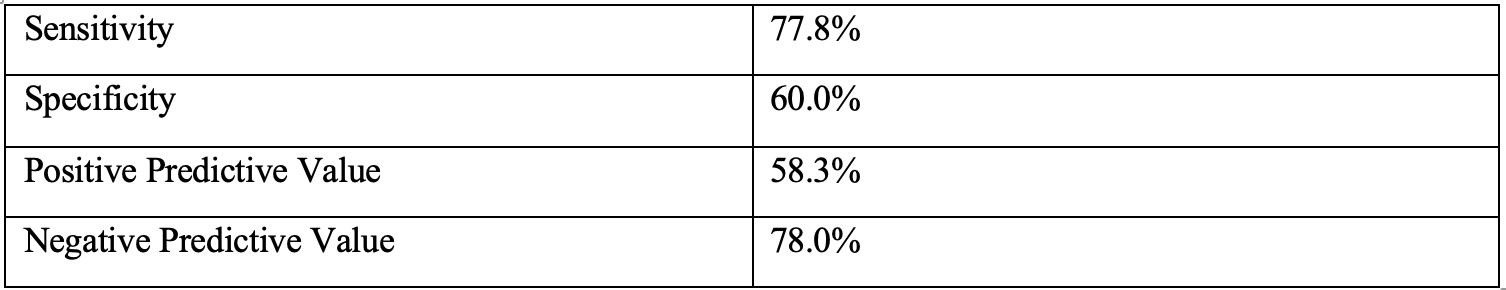
Design/Methods: A retrospective cohort study was conducted of youth aged 10 to 18 years, presenting to the ED between July 2020 and May 2022, who underwent routine suicide screening with the validated Ask Suicide Screening Questions (ASQ). Youth with a ‘positive’ screen were asked to self-report substance use history. ED return rate for mental health concerns, psychiatric admission rate, and UDS collection was determined at 6 months after the index visit. Substance use reporting by patients with and without an ED mental health return visit were compared using Fisher’s exact test of proportions. The association between self-reported substance use and ED mental health return was examined with simple logistic regression. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated.
Results:
During the study period 640 patients screened at-risk for suicide on the ASQ and completed a secondary risk assessment survey; 74 (11.6%) youth re-presented to the ED for an acute mental health concern, and 43 UDS samples (58.1% of visits) were collected. Of those with UDS samples collected, 35 (81.4) required a mental health admission. Among UDS samples, 18 (41.9%) were positive, and of those 14 (77.8%) were positive by self-report. UDS had moderate sensitivity (77.8%) and specificity (60.0%) when compared to self-report. For self-reported substance use the positive predictive value was 58.3% and negative predictive value was 78.9% compared to UDS. The odds of having a positive UDS were 4.20 times higher (95% CI:1.23, 14.39) among youth who self-reported any substance use compared to youth who denied prior substance use.
Conclusion(s): Patients reporting prior substance use had increased odds of a positive UDS. The utility of UDS was low for youth who denied substance use or abuse. Self-report of substance use or abuse among patients at-risk for suicide may be as reliable as UDS in the ED.