Medical Education: Resident
Medical Education 7: Resident 2
550 - Longitudinal Email-Based ECG Interpretation Curriculum for Pediatric Residents
Publication Number: 550.229

Margaret Van Der Bosch, MD (she/her/hers)
Resident
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background:
Electrocardiograms (ECGs) are frequently obtained tests in pediatric medicine that may be ordered for a broad variety of presentations. Interpretation of ECGs is made more complicated in pediatric medicine by the changing physiology of the heart as children age, and specific pediatric training in ECG interpretation is vital. However, exposure to ECG education both in medical school, which is largely adult focused, and in residency is highly variable. In a 2022 survey, less than half of responding pediatric residents at the University of Colorado (CU) reported feeling confident in ECG interpretation skills.
Objective:
This study aims to improve access to ECG interpretation training and pediatric resident ECG literacy at CU utilizing a longitudinal email-based curriculum.
Design/Methods:
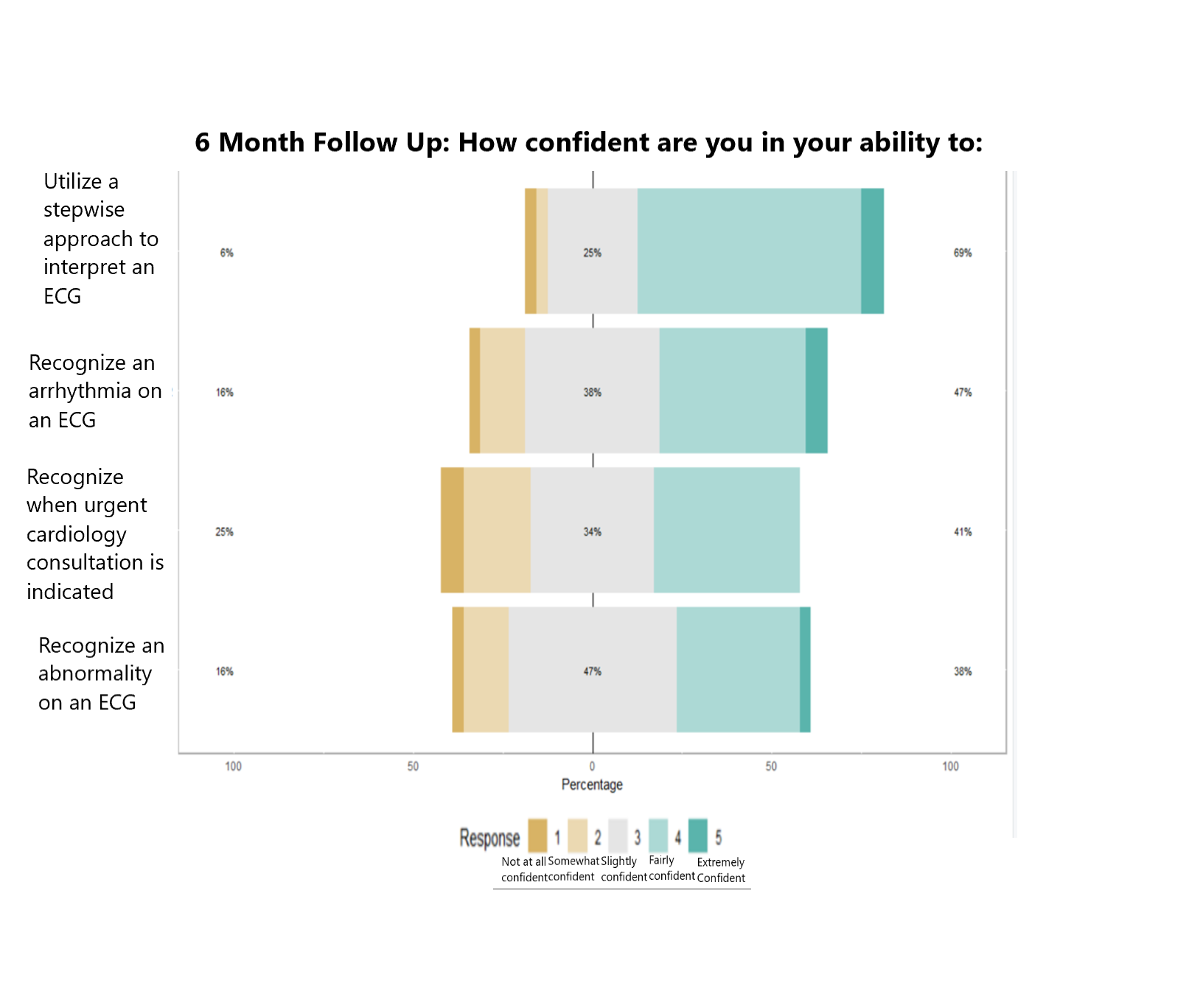
A pre-survey was administered to the CU pediatric and internal medicine/pediatrics residents to ascertain baseline comfort with ECG interpretation. They were asked to rate confidence in their ability to utilize a stepwise approach to interpret ECGs, to recognize an arrhythmia or other abnormality, and to know when to call urgent cardiology consultation. Residents were then twice monthly emailed a clinical vignette with an associated ECG and multiple choice question. After submitting their answer, residents were taken to a webpage with an explanation of the answer and key concepts demonstrated in each scenario. After six months, a follow up survey was administered asking residents to again rate their confidence in the same four skills. Responses were collected in a deidentified manner using REDCap. Descriptive statistics and linear regression analysis were used to understand how exposure to twice monthly practice correlated with changes in confidence in ECG interpretation skills.
Results:
60 residents participated in the pre-survey, and 75 participated in at least one clinical vignette. At the 6 month follow up survey (n=40), confidence in ability to use a stepwise approach increased by 27 percent (p-value 0.03) and in ability to recognize arrhythmias by 17 percent (p-value 0.02). There was no significant difference in confidence in ability to identify abnormalities or to know when urgent cardiology consultation is indicated. 83 percent of responding residents reported receiving no other formal ECG education during this time period.
Conclusion(s):
Pediatric ECG interpretation is a complex skill. The longitudinal email-based curriculum effectively increased both exposure to ECG training and resident confidence in ECG interpretation skills at the University of Colorado..png)