Endocrinology: All areas
Endocrinology 2
199 - New onset diabetes in children during the COVID-19 Pandemic: An assessment of biomarkers and psychosocial risk factors at play in Mississippi
Publication Number: 199.214

Josephine Stout, MD (she/her/hers)
Pediatric Critical Care Fellow
University of Mississippi School of Medicine
Jackson, Mississippi, United States
Presenting Author(s)
Background:
The COVID-19 pandemic has shown a rise in the incidence of pediatric diabetes. Studies have indicated increased likelihood of children with COVID-19 infection developing diabetes, however, there remains a paucity of data regarding possible factors affecting the pediatric population during the pandemic, such as infection, obesity, vitamin D deficiency, etc., and behavioral changes due to lockdowns and virtual learning.
Objective:
To investigate associations between the COVID-19 pandemic and new onset diabetes in children.
Design/Methods:
Children aged 1-18 years admitted to the hospital with new-onset-diabetes between March 2020 and December 2021 were eligible. Leptin, CRP, cytokines IL-1b, IL-6, and TNF-alpha, SARS-CoV2 IgM and IgG antibodies assays were completed for each enrolled patient. Demographic data, vital signs and pertinent laboratory data were gathered from the electronic medical record. Families completed a behavioral questionnaire at the time of enrollment. Univariate and multiple binary logistic regression were used to analyze results.
Results:
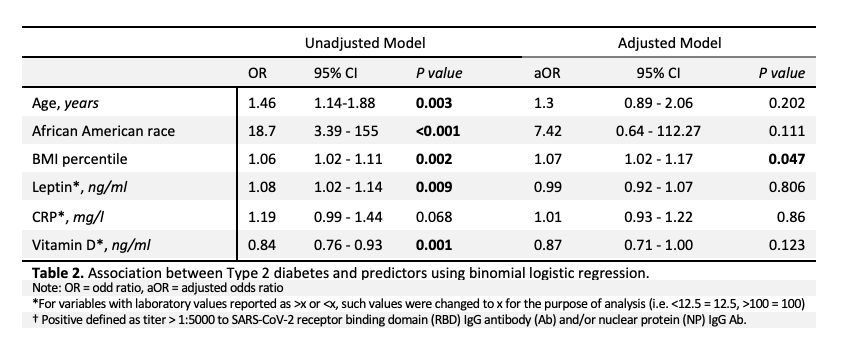
Of the children with complete data sets (N = 58), 19 (33%) had positive SARS-CoV-2 IgG antibodies (Ab) while 39 (67%) were IgG Ab negative, and 18 (31%) had type 1 diabetes mellitus (T1DM), while 36 (62%) had type 2 diabetes mellitus (T2DM). There were 29 (53.7%) in DKA on admission. Those with T2DM were older (median age 14.0 vs 10.5 years, p=0.004), majority African American (94.4 vs 44.4%, p< 0.001) and had a higher median BMI percentile (99.2 vs 67.6 %ile, p< 0.001), lower Vitamin D (median 12.8 vs 24.5 ng/mL, p< 0.001), and higher Leptin (median 19.9 vs 3.45 ng/mL, p< 0.001) and CRP (median 4.9 vs 0.40 mg/L, p< 0.001). Binary logistic regression showed that for every percentile increase in BMI, the odds of having T2DM are 1.07 times greater (adjusted odds ratio 1.07 [95% CI 1.02-1.17], p=0.047) (Tables 1 and 2). Of note, there were no significant differences in survey responses (Table 3).
Conclusion(s):
This study highlighted few differences in predictive indicators between children who were COVID-19 Ab positive vs Ab negative. There were differences in predictors of T1DM vs T2DM, however, all except BMI percentile lost significance on multivariate analysis. The high percentage of children presenting in DKA may indicate delay in seeking medical care due to the pandemic. Further work with greater statistical power is needed to elaborate correlations between psychosocial factors & SARS-CoV-2 infection related biomarkers with incident diabetes in children.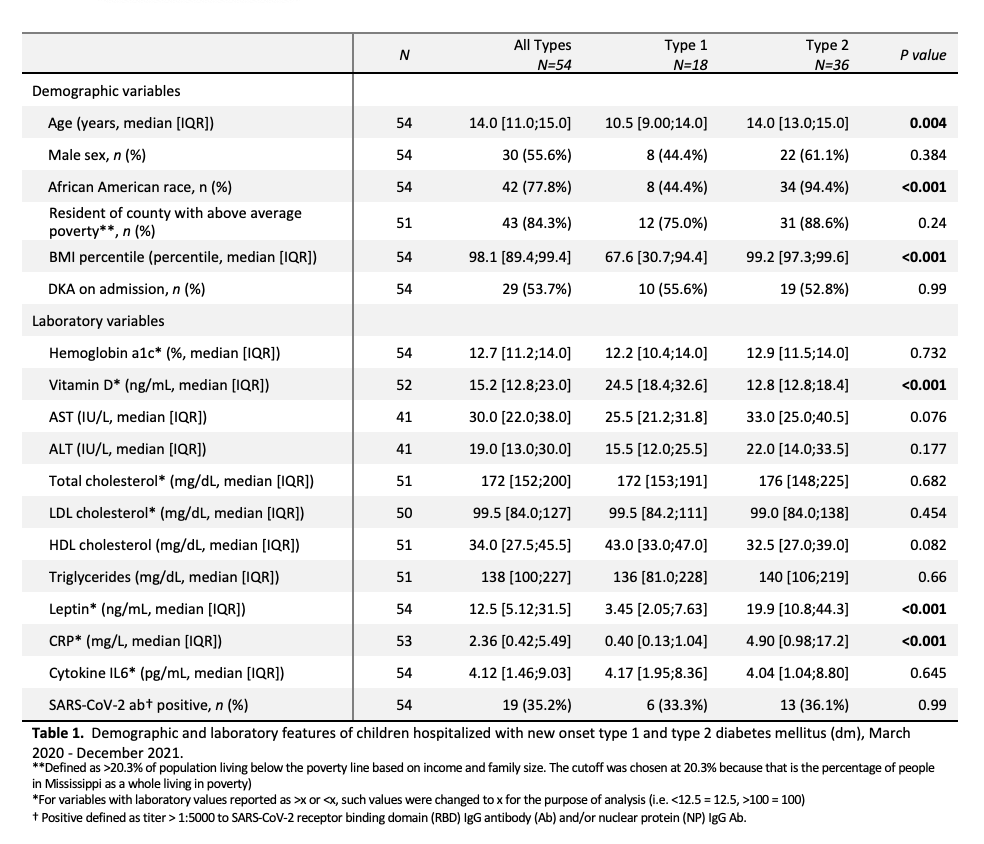
.png)
