Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 2
675 - Viral Testing Decreases Antibiotic Treatment and Hospitalization Duration of Febrile Infants
Publication Number: 675.241
- GE
Guliz Erdem, MD (she/her/hers)
Professor
Nationwide Children's Hospital
columbus, Ohio, United States 
Cristina Tomatis Souverbielle, MD (she/her/hers)
assistant professor
Nationwide Children's Hospital
Worthington, Ohio, United States
Presenting Author(s)
Co-Author(s)
Background:
AAP febrile infant management guidelines suggest that viral infections could be associated with reduced frequency of invasive bacterial infections (IBI) in infants. However, clinical care variation continues to exist, particularly in those between 4-8 weeks of age who have a viral infection.
Objective:
We have been using divisional “low-risk” criteria for several years and wanted to assess their use in the “real-world” setting in hospitalized infants for duration of antimicrobial treatment, length of stay (LoS) and IBI rates.
Design/Methods:
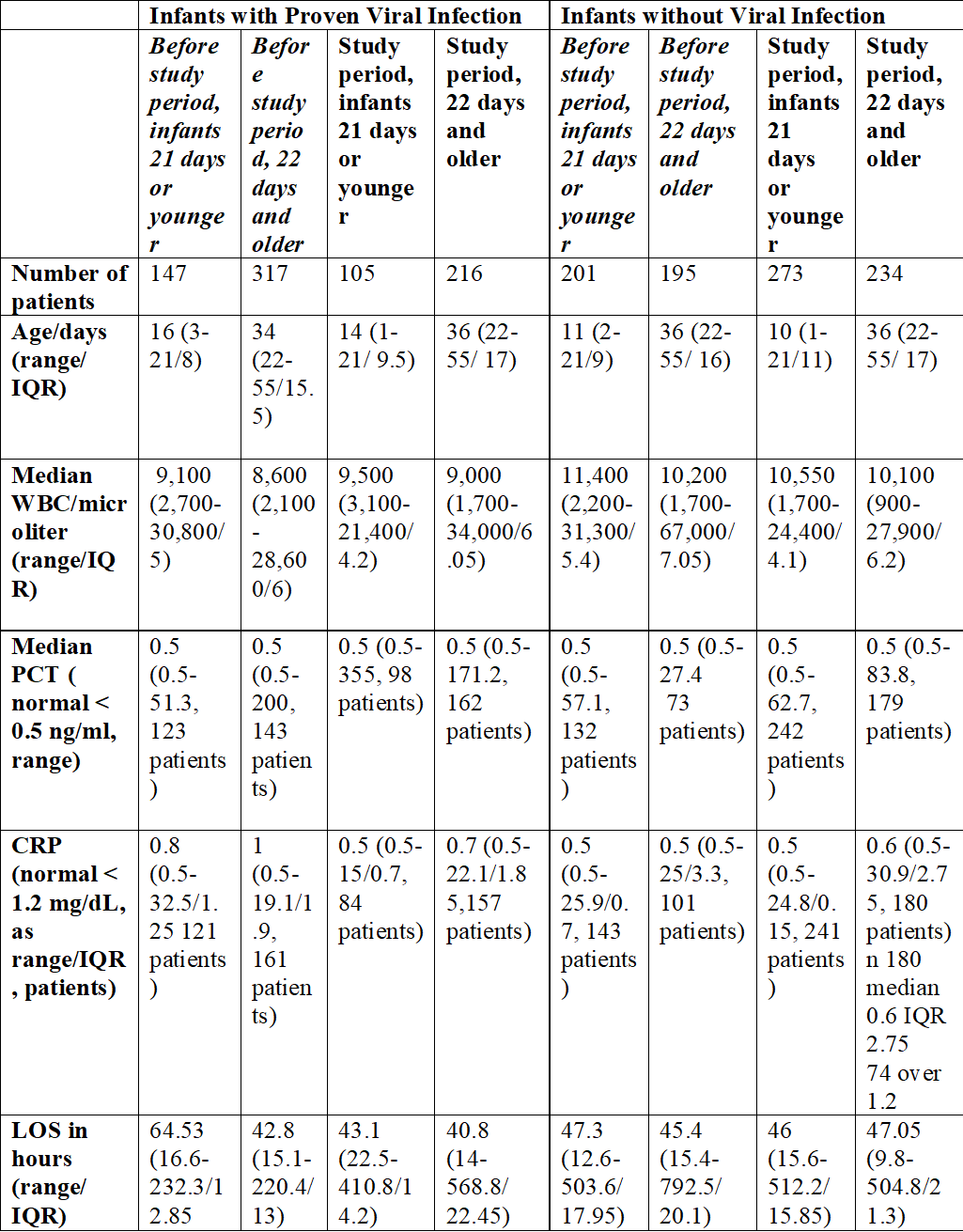
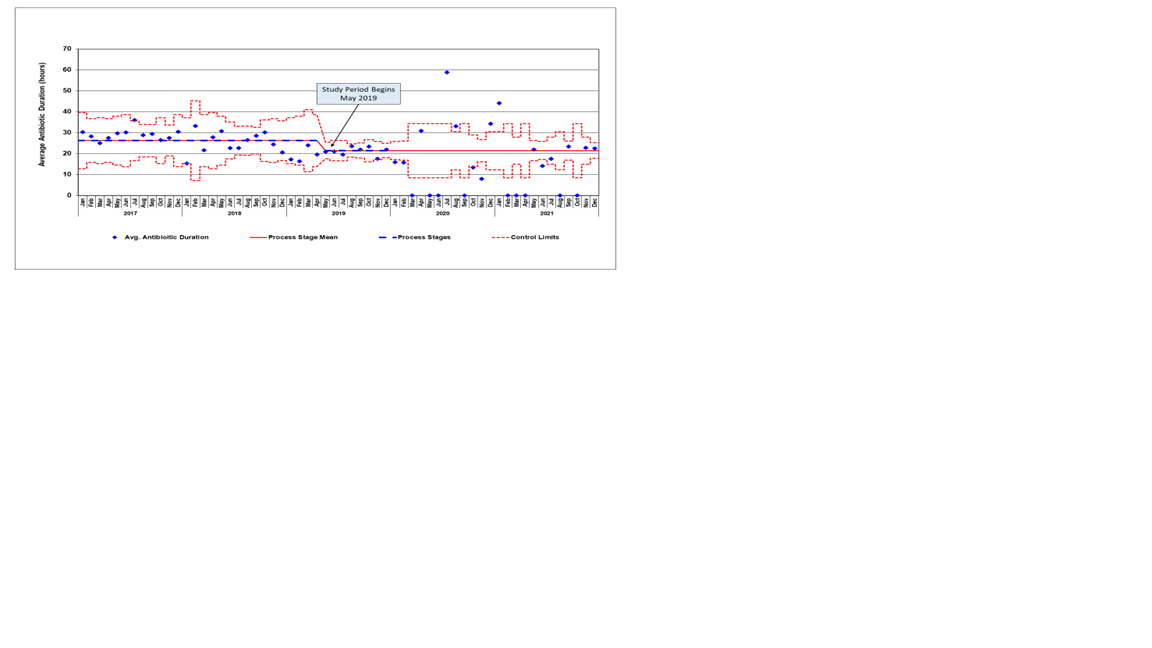
We created a guideline to stop antimicrobial treatment at 24 hours if bacterial cultures are negative and viral testing is positive. The primary outcome was to decrease the treatment duration in infants less than 8 weeks of age who had enterovirus, parechovirus, or respiratory viruses detected by PCR. The secondary outcome was to decrease the treatment duration and LoS in all infants regardless of viral test results. We monitored IBIs and 72-hour revisits requiring admission as balancing measures. The pre-study baseline period was 1/1/2017 to 4/30/2019 and the study period was 5/1/2019 to 7/1/2021. IBI was defined as a positive blood or CSF culture with a known pathogen. Control charts were used to assess the impact of the interventions.
Results:
We studied 1688 infants including 860 (51%) before and 828 (49%) after the implementation of the guidance. Groups were evaluated based on age and presence of an identified viral infection. 321 infants with during the study period had a viral infection. During the study period, median treatment duration in infants with a viral infection decreased from 31.5 hours to 24.8 hours in infants < 21 days (p < 0.001), and decreased from 26.0 hours to 19.7 hours in infants 22-56 days of age (p < 0.001). Median LoS decreased in all but patients >21 days of life with no identified viral infection. Adherence to the pathway led to a sustained reduction in antimicrobial administration for 24 months. IBI rates were higher overall in patients without identified viral infection (5.1% vs 2.4% in patients with viral infection).
Conclusion(s):
Use of viral testing was associated with significant decrease in antimicrobial duration in febrile infants with no observed differences in outcomes. We showed significantly higher rates of IBI in infants >21 days who did not have a proven viral etiology. This may have further importance in decision making in terms of admission, discharge, and antimicrobial treatment. The benefits of shortened antimicrobial duration and hospitalization course may offset the concerns for additional viral work up.